Active Ingredients: Are Generic Drugs Really the Same as Brand-Name Drugs?

Every year, millions of people in the U.S. switch from brand-name medications to generics - not because they want to, but because their insurance won’t cover the brand. You’re handed a little white pill instead of the colorful one you’re used to, and suddenly you wonder: is this really the same thing?
Same active ingredient, same effect
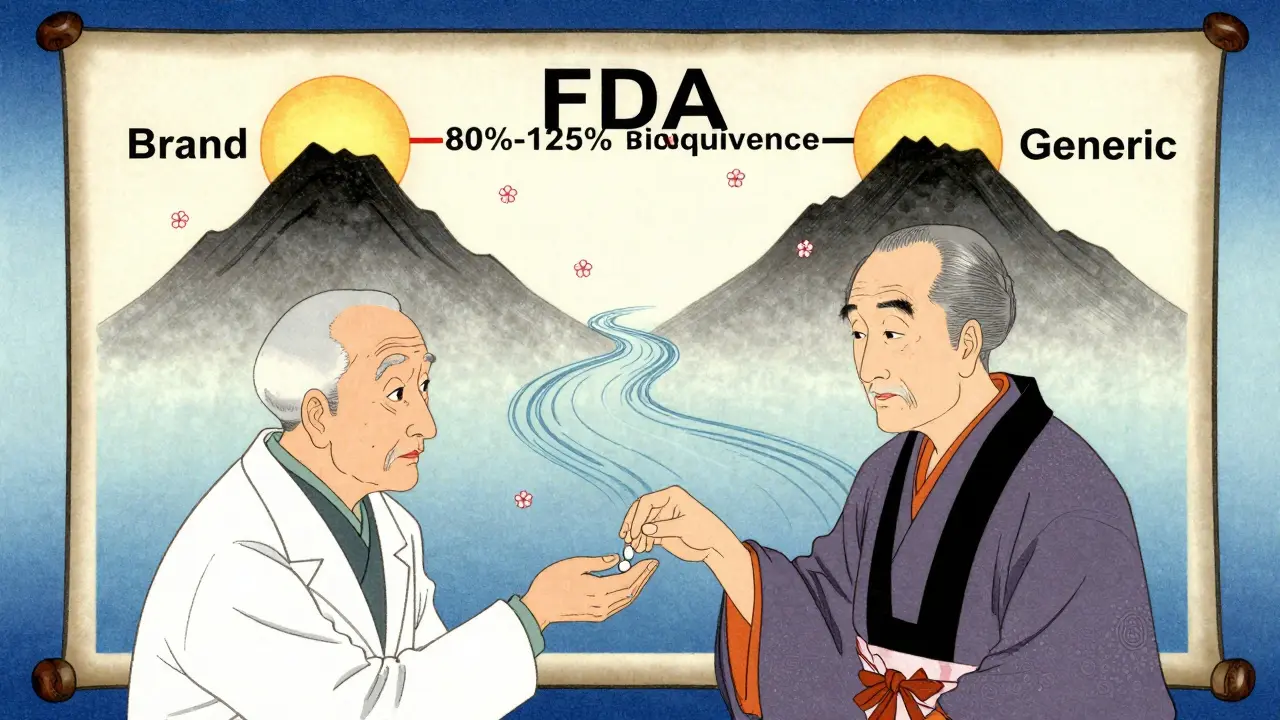
The answer is yes - if it’s FDA-approved. Generic drugs contain the exact same active ingredient as their brand-name counterparts. That means if your brand-name blood pressure pill has amlodipine besylate as its active ingredient, so does the generic version. Same molecule. Same chemistry. Same way it works in your body.The FDA doesn’t just take a manufacturer’s word for it. To get approved, a generic drug must prove it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand. This is called bioequivalence. The standard? The generic’s absorption must fall within 80% to 125% of the brand’s. That’s not a wide margin - it’s tight enough to ensure you get the same clinical result.
Think of it like two identical engines. One is built by the original manufacturer. The other is made by a different company, but uses the same blueprints, same materials, same tolerances. They run the same. The only difference? The paint job and the price tag.
Why are generics so much cheaper?
Brand-name drugs cost a fortune because the company had to pay for years of research, clinical trials, and marketing. They got a patent to protect their investment - usually 20 years from the date it was filed. Once that patent expires, other companies can make the same drug without repeating all that expensive work.That’s thanks to the 1984 Hatch-Waxman Act. It created a shortcut called the Abbreviated New Drug Application (ANDA). Generic makers don’t need to run new safety trials. They just need to prove their version works the same way. That cuts development costs by 80-90%. Those savings get passed on.
Take metformin, the go-to drug for type 2 diabetes. The brand name, Glucophage, used to cost over $350 for a 30-day supply. The generic? Around $4. Amlodipine (Norvasc) went from $400 to $2. These aren’t outliers. According to Brown University Health, generics cost, on average, 85% less than brand-name versions.
What’s different? (Spoiler: It’s not the medicine)
You might notice the generic pill looks different - different color, shape, size, even taste. That’s because the inactive ingredients are not required to match. These include fillers, dyes, binders, and preservatives. They make up most of the pill’s weight - sometimes over 90% - but they don’t affect how the drug works.That’s also why some people report side effects after switching. A 2023 GoodRx survey of 5,000 patients found that 12% noticed mild changes after switching to generics. Most of those were stomach upset, headaches, or dizziness. In rare cases, someone might be sensitive to a dye or filler in the generic version - like FD&C Red No. 40 or lactose. But these reactions are uncommon, happening in fewer than 1 in 2,000 switches, according to FDA adverse event data.
And here’s the thing: brand-name drugs use inactive ingredients too. The difference is, you’ve been used to that specific combination. When you switch, your body notices a change - even if it’s not the active ingredient causing it.
Do generics work as well? The science says yes
A 2019 study in JAMA Internal Medicine looked at over 3.5 million patients taking generics versus brand-name drugs for conditions like high blood pressure, diabetes, epilepsy, and depression. The results? No meaningful difference in outcomes. Blood pressure dropped the same. Blood sugar stabilized the same. Depression symptoms improved equally.Dr. Aaron Kesselheim, a professor at Harvard Medical School, reviewed 47 high-quality studies on cardiovascular generics in 2022. His conclusion? No evidence that brand-name drugs performed better.
Even for tricky drugs like warfarin (a blood thinner) or levothyroxine (for thyroid issues), the FDA says approved generics are safe and effective. These are called narrow therapeutic index (NTI) drugs - meaning small changes in dosage can matter. But the FDA still requires them to meet the same 80%-125% bioequivalence standard. In practice, most patients switch without issue. Some doctors prefer to keep patients on the same version - not because generics are less effective, but to avoid any confusion.
What about quality? Are generics made in shoddy factories?
No. The FDA inspects every facility - whether it makes brand-name or generic drugs - using the same strict rules. All must follow Current Good Manufacturing Practices (cGMP). In 2022, the FDA conducted over 3,500 inspections of drug plants worldwide. About 12 facilities in India and China were flagged that year for quality issues - that’s 0.5% of total production. Those plants were blocked from shipping to the U.S. until they fixed the problems.The same factories that make brand-name drugs often make generics too. Teva, Mylan, and Sandoz - three of the biggest generic makers - also produce brand-name drugs under different labels. The difference isn’t in the facility. It’s in the price tag.
Why do some doctors still hesitate?
Most doctors trust generics. The American College of Physicians says the evidence overwhelmingly supports their use. But some still hesitate - especially with older patients or those on multiple medications. Why? Because appearance changes can cause confusion.If you’re taking five pills a day, and one changes color every few months, it’s easy to get mixed up. That’s why pharmacists are trained to explain the switch. A 2022 UC Health study found that 95% of patients understood the concept after a two-minute conversation.
Also, some patients report feeling worse after switching - even when labs show no change. That’s often psychological. If you believe the generic is “inferior,” your brain can amplify minor side effects. It’s not the drug. It’s the expectation.
How to make the switch confidently
If your prescription is switched to a generic:- Ask your pharmacist: “Is this FDA-approved as therapeutically equivalent?” They can show you the FDA’s Orange Book listing.
- Check the pill’s appearance. Take a photo if you’re worried about future changes.
- Monitor how you feel for the first 2-4 weeks. Most side effects, if any, show up early.
- Don’t panic if you feel slightly off. Give it time. If symptoms persist, talk to your doctor - but don’t assume it’s the generic’s fault.
- Use tools like GoodRx or Drugs.com to compare prices and read patient reviews.
Most insurance plans now require you to try the generic first. If it doesn’t work - and that’s rare - your doctor can write “Do Not Substitute” on the prescription. But 92% of the time, the generic works just fine.
The big picture: Generics save billions
In 2022 alone, generics saved the U.S. healthcare system $313 billion. Over the past decade, that adds up to $2.2 trillion. That’s money kept in patients’ pockets, not spent on unnecessary brand-name premiums.By 2028, generics are expected to make up 95% of all prescriptions. Why? Because more brand-name drugs are losing patents. Big ones like Eliquis and Stelara - which together brought in nearly $20 billion in 2022 - are now open to generic competition.
The system works. Generics aren’t cheaper because they’re worse. They’re cheaper because the system was designed to make them that way - without sacrificing safety or effectiveness.
So when you see that little generic pill, remember: it’s not a compromise. It’s the same medicine, at a fraction of the cost. And for most people, that’s exactly what they need.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies involving millions of patients show no difference in clinical outcomes for conditions like high blood pressure, diabetes, depression, and more.
Why do generic pills look different?
By law, generic drugs can’t look exactly like the brand-name version - that’s to avoid trademark infringement. So manufacturers change the color, shape, size, or markings. These differences are only in the inactive ingredients - like dyes or fillers - which don’t affect how the drug works. The active ingredient is identical.
Can generic drugs cause more side effects?
Rarely. Most side effects are caused by the active ingredient, which is the same in both versions. But some people may react to a different inactive ingredient - like a dye or filler - in the generic. This happens in fewer than 1% of cases. If you notice new symptoms after switching, talk to your doctor. It’s usually not the drug’s fault, but it’s worth checking.
Are generic drugs made in lower-quality facilities?
No. The FDA inspects all drug manufacturing facilities - whether they make brand-name or generic drugs - using the same strict standards. All must follow Current Good Manufacturing Practices (cGMP). In fact, many brand-name companies also produce generics under different labels. The difference is cost, not quality.
Should I avoid generics for critical medications like blood thinners or thyroid drugs?
No. The FDA approves generics for even the most sensitive drugs - including warfarin, levothyroxine, and anti-seizure medications. These are called narrow therapeutic index (NTI) drugs, and they still must meet the same 80%-125% bioequivalence standard. While some doctors prefer consistency (sticking with one version), there’s no evidence that generics are less safe or effective. If your doctor is concerned, they can write “Do Not Substitute” on the prescription.
Why do pharmacies automatically switch to generics?
Because it’s legal, safe, and saves money - for you and the system. In 49 U.S. states, pharmacists can substitute FDA-approved generics unless the doctor says “Do Not Substitute.” Insurance companies require it too - they won’t pay full price for a brand if a generic is available. This system saves billions each year without compromising care.
Ryan Barr
January 6, 2026 AT 18:20Isaac Jules
January 7, 2026 AT 17:33Pavan Vora
January 9, 2026 AT 02:32Indra Triawan
January 10, 2026 AT 16:36Susan Arlene
January 12, 2026 AT 11:59Joann Absi
January 12, 2026 AT 19:43Mukesh Pareek
January 14, 2026 AT 00:26Ashley S
January 14, 2026 AT 23:45Jeane Hendrix
January 16, 2026 AT 04:01Rachel Wermager
January 17, 2026 AT 11:21Tom Swinton
January 19, 2026 AT 06:39Leonard Shit
January 20, 2026 AT 22:00