Acute Kidney Injury: Sudden Loss of Function and Recovery
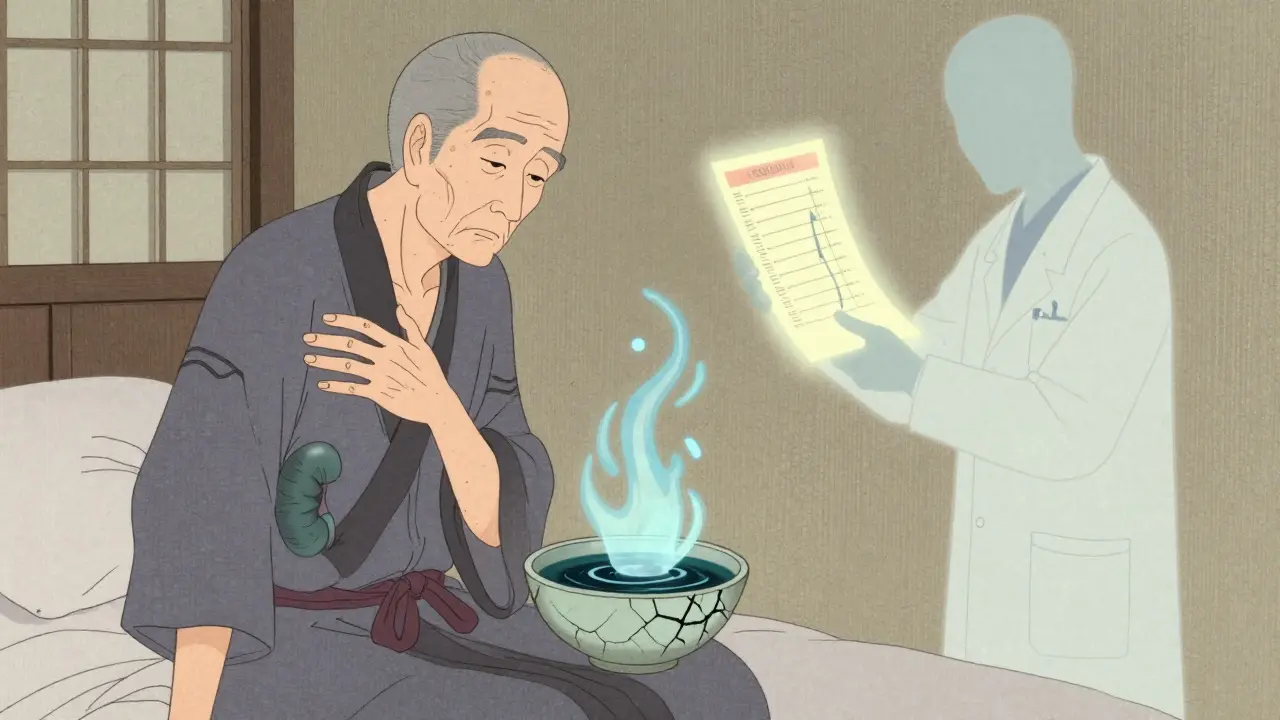
Acute Kidney Injury (AKI) doesn’t announce itself with a siren. It creeps in quietly-sometimes after a bad bout of food poisoning, a high fever, or even just skipping fluids for a day. One moment you feel a little tired; the next, your body starts holding onto water, your urine drops, and your blood tests show something’s wrong with your kidneys. This isn’t chronic kidney disease. This is sudden. Fast. And if you don’t act, it can turn deadly.
What Exactly Happens When Your Kidneys Shut Down?
Your kidneys don’t just make urine. They clean your blood, balance your electrolytes, control your blood pressure, and remove waste. When AKI hits, that system slows or stops-sometimes in just hours. The medical definition is simple: a rapid rise in creatinine (a waste product your kidneys normally filter out) or a drop in urine output. According to KDIGO guidelines, if your creatinine jumps by 0.3 mg/dL in 48 hours, or falls by 50% from your normal level over a week, you’re in AKI territory. But here’s the catch: you might not feel it. About 22% of people with AKI have no symptoms at all. Their doctors catch it during routine bloodwork. That’s why, if you’re hospitalized, especially in the ICU, your creatinine is checked every day. If you’re over 65, have diabetes, or take blood pressure meds, you’re at higher risk-and you need to be watched closely.Three Main Causes, Three Different Treatments
AKI doesn’t have one cause. It has three, and knowing which one you’re dealing with changes everything.- Prerenal (60-70% of cases): Your kidneys aren’t damaged-they’re just not getting enough blood. This happens with severe dehydration, heavy bleeding, heart failure, or low blood pressure. A 70-year-old who hasn’t drunk water in two days after vomiting? That’s prerenal. Treatment? Fluids. Fast. A liter or two of IV saline often brings kidney function back in 24 hours.
- Intrarenal (25-35%): This is where the kidney tissue itself gets hurt. The most common cause? Acute tubular necrosis (ATN), often from medications like antibiotics (aminoglycosides), contrast dye used in CT scans, or sepsis. Glomerulonephritis and lupus can also trigger this. Stopping the toxin is step one. For autoimmune causes, steroids or plasmapheresis may be needed. Recovery takes weeks, not days.
- Postrenal (5-10%): Something’s blocking the urine flow. In men over 60, that’s often an enlarged prostate. In others, it’s kidney stones or a tumor. If the blockage isn’t cleared, pressure builds and kills kidney cells. A simple ultrasound can spot this. A stent or catheter? Usually fixes it in hours.
When Symptoms Show Up-And When They Don’t
Some people know something’s wrong. They notice swelling in their legs, feel out of breath from fluid in their lungs, or get confused because toxins are building up in their brain. Fatigue hits hard-75% of patients report it. Nausea? Common. Flank pain? Happens in about a quarter of cases. Chest pain? That’s a red flag-could mean pericarditis from uremia. But again, don’t wait for symptoms. Many cases are silent. That’s why labs matter more than how you feel. A creatinine of 1.8 mg/dL might not sound scary-but if your normal is 0.8, that’s a 125% jump. That’s stage 2 AKI.What Happens If It’s Not Treated?
Untreated AKI doesn’t just linger-it escalates. Fluid overload can lead to pulmonary edema. Potassium spikes above 5.5 mEq/L? That can trigger a fatal heart rhythm. Acid builds up. Your blood turns acidic. Your heart struggles. Your lungs fill. Your brain fogs. And even if you survive, the damage doesn’t always heal. One in five AKI survivors ends up with chronic kidney disease within a year. Each episode raises your risk of needing dialysis later by over eight times. That’s not a small risk. It’s life-altering.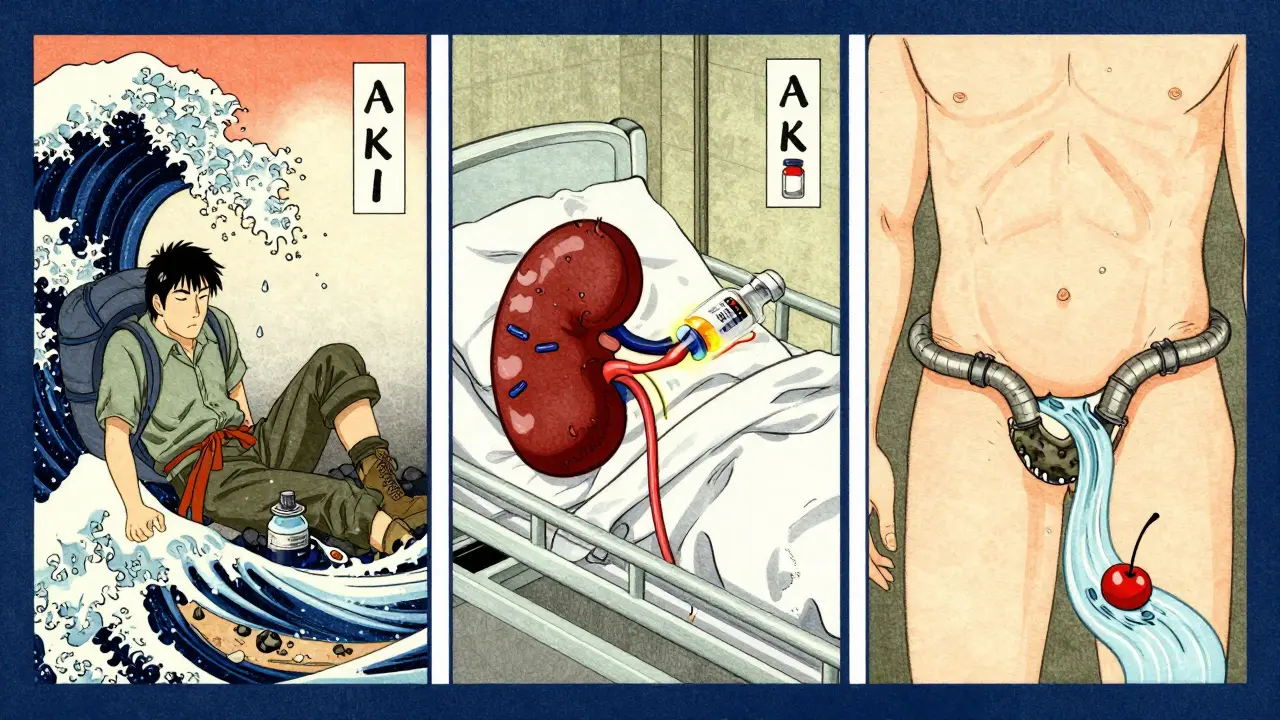
Recovery: It’s Not Guaranteed
You might think, “If I get treated, I’ll bounce back.” But recovery isn’t automatic.- Prerenal AKI? 70-80% recover fully in under 10 days.
- Intrarenal AKI? Only 40-60% recover fully. Some get better but never return to baseline.
- Severe ATN with no urine for two weeks? Only 20-30% fully recover.
How Doctors Diagnose It
It starts with blood and urine tests. Creatinine, BUN, electrolytes. Then comes the fractional excretion of sodium (FeNa). If it’s under 1%, your kidneys are conserving fluid-classic prerenal. Over 2%? You’ve got internal damage. Ultrasound is the go-to imaging tool. It checks for swelling, size, and blockages. A CT scan with contrast? Only if absolutely necessary-because contrast dye can cause more kidney injury. But if they suspect stones, CT urography is 95% accurate. Newer tools are emerging. Biomarkers like NGAL and TIMP-2/IGFBP7 can predict AKI 24 to 48 hours before creatinine rises. Some hospitals are already using them in ICUs. They’re not perfect-but they’re getting better.Treatment: Fast, Targeted, and Personal
There’s no one-size-fits-all fix.- Prerenal: Fluids. Simple. Effective. Most cases resolve within 48 hours.
- Intrarenal: Stop the bad meds. Treat infections. Use steroids for inflammation. Plasmapheresis for rare autoimmune cases.
- Postrenal: Unblock it. Stent. Catheter. Surgery. Relief is often immediate.
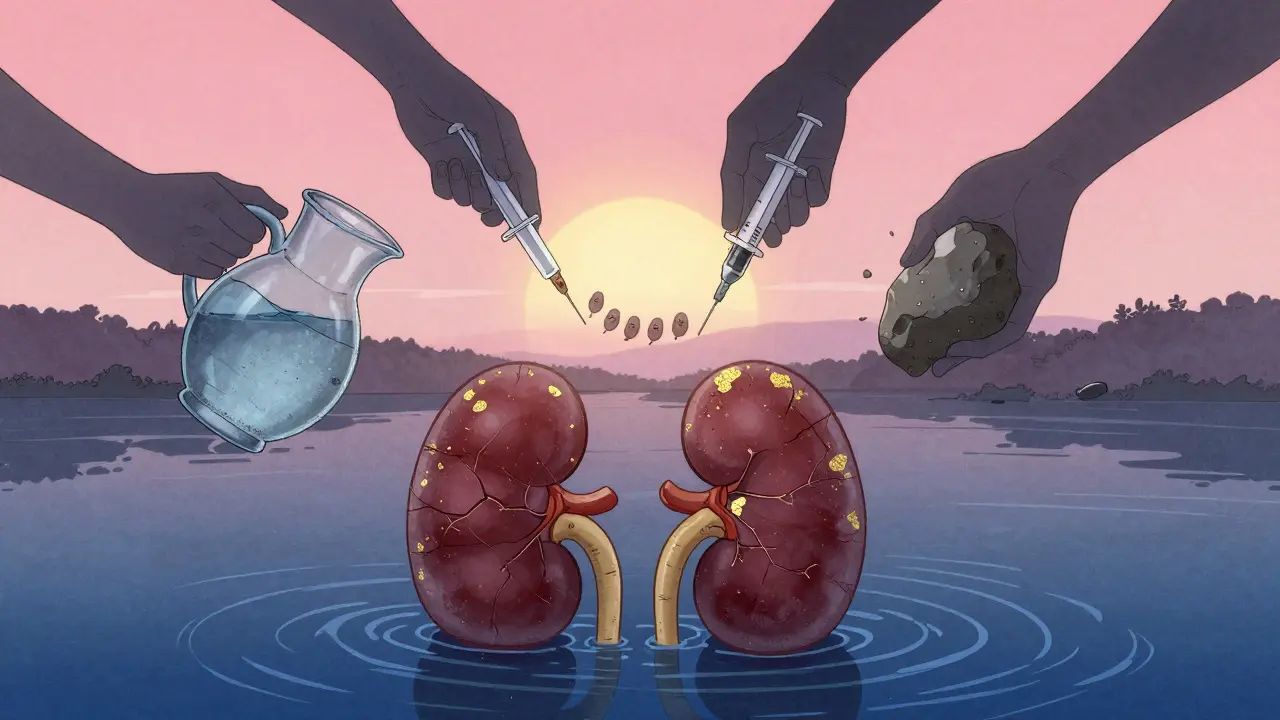
What You Can Do to Prevent It
You can’t control sepsis or a heart attack. But you can control a lot.- Stay hydrated. Especially if you’re sick, sweating, or on diuretics.
- Avoid NSAIDs like ibuprofen if you have kidney disease or are dehydrated.
- Know your baseline creatinine. Ask your doctor for a copy of your last blood test.
- Don’t skip follow-ups after hospital discharge. 45% of AKI survivors need a nephrologist within six months.
- Ask about contrast dye risks before a CT scan. If you’re at risk, your doctor can use a safer agent or pre-hydrate you.
The Future: AI, Biomarkers, and Early Alerts
Hospitals are starting to use AI to predict AKI before it happens. By analyzing your vitals, meds, and lab trends, algorithms can flag risk 12 to 24 hours in advance. One project projected a 20-30% drop in AKI cases if these systems are widely adopted. The STARRT-AKI trial showed that starting dialysis earlier in severe cases cuts 90-day death rates by 9%. That’s huge. And the cost? AKI adds $10,000 to $15,000 per hospital stay. In the U.S. alone, it costs $10 billion a year. That’s not just money-it’s time, stress, and lost life.Final Thought: Time Is Kidney
Acute Kidney Injury isn’t a slow burn. It’s a fire. The window to save your kidneys is narrow-often just 6 to 12 hours after the insult. If you’re hospitalized, ask: “Am I being monitored for AKI?” If you’re home and feel off after illness, get your creatinine checked. Don’t wait for swelling or confusion. Don’t assume you’re fine because you’re peeing. Your kidneys don’t shout. They whisper. And if you don’t listen, they might stop speaking altogether.Can acute kidney injury be reversed completely?
Yes, in many cases-especially if caught early and the cause is prerenal (like dehydration or low blood pressure). Around 70-80% of prerenal AKI cases fully recover within a week. Intrarenal cases, like those from medication damage or sepsis, have a lower recovery rate-40-60%-and may leave some lasting damage. If dialysis was needed, only about 25% regain full kidney function within three months.
What are the first signs of acute kidney injury?
The earliest and most common sign is reduced urine output-less than 400 mL per day (oliguria) or even less than 100 mL (anuria). But some people keep producing normal urine. Other early signs include swelling in the legs, fatigue, nausea, confusion, or shortness of breath. Often, though, the first sign is a blood test showing a rise in creatinine-before any symptoms appear.
Can drinking more water prevent acute kidney injury?
For prerenal AKI caused by dehydration, yes-staying hydrated is one of the best protections. But drinking more won’t help if the cause is something else, like sepsis, kidney stones, or toxic drugs. If you’re already sick, vomiting, or on diuretics, you need more than just water-you need medical evaluation. Don’t self-treat. If you’re at risk, talk to your doctor about hydration plans.
Is acute kidney injury the same as chronic kidney disease?
No. AKI is sudden and often reversible. Chronic kidney disease (CKD) is gradual, lasting three months or more, and usually progressive. But AKI can lead to CKD. About 23% of AKI survivors develop stage 3 or worse CKD within a year. Each episode increases your long-term risk of kidney failure.
What medications should I avoid if I’m at risk for AKI?
Avoid NSAIDs (ibuprofen, naproxen), certain antibiotics like aminoglycosides (gentamicin), and contrast dye used in CT scans if you’re dehydrated or have existing kidney issues. Diuretics and some blood pressure meds (ACE inhibitors, ARBs) can also worsen AKI in vulnerable people. Always check with your doctor before taking new meds, especially during illness or hospital stays.
How long does recovery from AKI take?
It varies. Prerenal AKI often resolves in 1-7 days. Intrarenal AKI from tubular damage can take 2-6 weeks. If you had severe injury or needed dialysis, recovery may take months-or never fully happen. Even after creatinine normalizes, many people feel fatigued for 3-6 months. Follow-up care is essential.
Can AKI come back after recovery?
Yes. Having one episode of AKI makes you more vulnerable to future ones. Your kidneys are scarred or weakened, even if they seem fine. Avoid dehydration, nephrotoxic drugs, and uncontrolled infections. Regular kidney checks and a healthy lifestyle reduce your risk of recurrence.
Do I need to see a kidney specialist after AKI?
Yes, if you had moderate to severe AKI, or if you’re over 65, diabetic, or had pre-existing kidney issues. About 45% of AKI survivors need a nephrologist within six months. They’ll monitor your kidney function, manage blood pressure, and help prevent progression to chronic disease.