Age Spot Check: How to Know if They're Harmless or Worry‑Worthy

Age Spot Risk Checker
Spot Characteristics
Please select the characteristics of your spot to determine its risk level.
Comparison Table
Key differences between harmless age spots and potential warning signs:
| Feature | Harmless Age Spot | Potential Warning Sign |
|---|---|---|
| Color | Uniform brown or tan | Variegated (brown, black, red, white, blue) |
| Border | Smooth, well-defined | Irregular, scalloped, fuzzy |
| Shape | Symmetrical | Asymmetrical |
| Size | Usually < 6 mm and stable | > 6 mm or rapid growth |
| Texture | Flat, smooth | Raised, scaly, crusted, or bleeding |
Risk Assessment Result
Enter spot characteristics above to assess risk level
Quick Take
- Age spots are usually harmless, flat, brown patches that develop from long‑term sun exposure.
- Watch for changes in size, shape, color, or texture - they may signal a problem.
- Four red‑flag signs (asymmetry, border irregularity, color variation, diameter >6mm) call for a professional look.
- Do a regular self‑exam and note any evolution; photograph spots for tracking.
- See a dermatologist promptly if any warning signs appear or if a spot bleeds, itches, or crusts.
Understanding whether your age spots are harmless or a sign of something more serious can feel confusing. This guide walks you through what they are, how to spot warning signs, and when to get expert help.
What Are Age Spots?
Age spots (solar lentigines) are small, flat, brown patches that appear on skin that’s been exposed to the sun. They’re usually harmless and develop over many years of UV radiation. Most people notice them after the age of 40, but they can show up earlier if sun damage has been intense.
Why They Appear: Sun Exposure and UV Index
Sun exposure is the primary driver of age spots. When ultraviolet (UV) rays penetrate the skin, they trigger melanin production, and over time the pigment settles into clusters that become visible as spots. The intensity of that exposure is measured by the UV Index, a scale from 0 (minimal) to 11+ (extreme). Higher UV Index values mean more melanin‑stimulating energy reaches your skin, speeding up the formation of age spots.
Typical Look of Harmless Spots
- Uniform brown or tan color, matching the surrounding skin tone.
- Even, well‑defined borders without ragged edges.
- Flat to the touch, no raised surface.
- Stable size - they don’t grow noticeably over months.
When all these characteristics line up, the spot is likely a benign age spot.
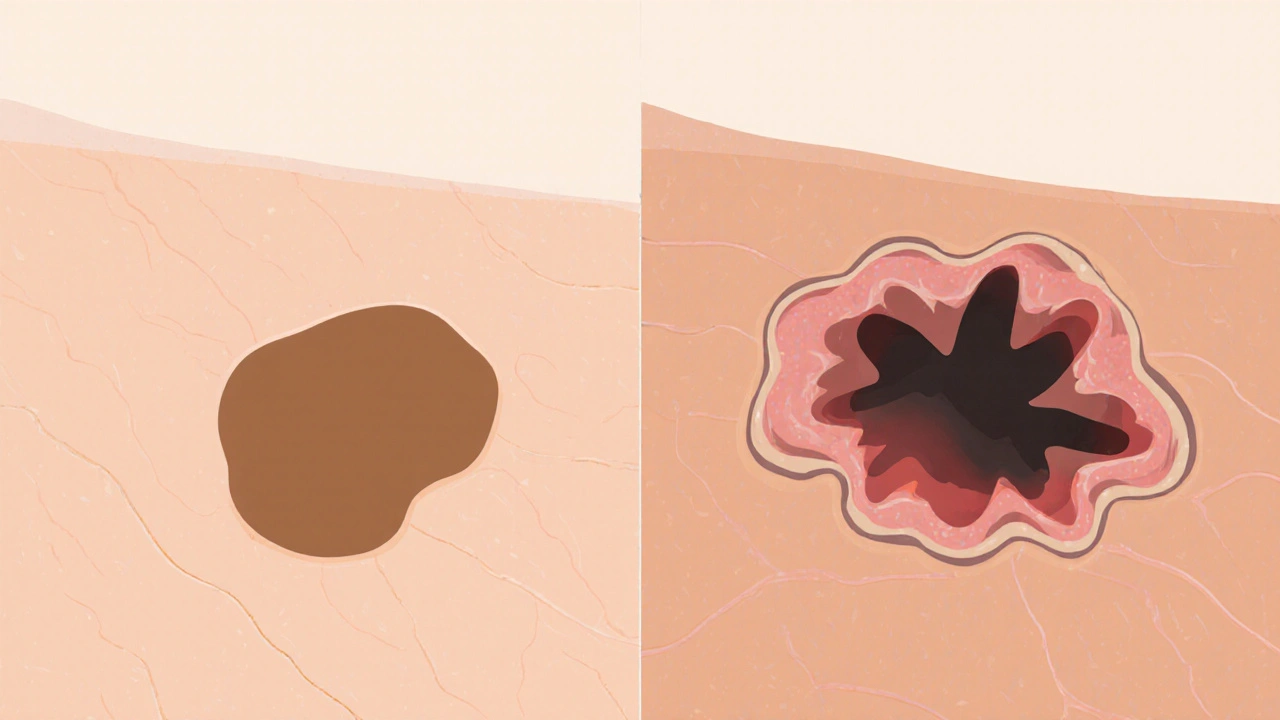
Red Flags: When a Spot Might Signal Something Serious
Even though most spots are harmless, a handful of features can hint at skin cancer or precancerous conditions. Keep an eye out for the following:
- Asymmetry - one half looks different from the other.
- Irregular, scalloped or fuzzy borders.
- Multiple colors (brown, black, red, white, or blue) within the same spot.
- Diameter larger than 6mm (about the size of a pencil eraser).
- Rapid growth, itching, bleeding, or crust formation.
If any of these appear, it’s time to consider the possibility of skin cancer. The three most common types are melanoma, a fast‑growing cancer that can spread to other organs, basal cell carcinoma (usually appears as a pearly or waxy bump), and actinic keratosis (a rough, scaly patch that can turn into squamous cell carcinoma). While not every red‑flag spot is cancer, these conditions share similar visual cues.
How to Self‑Examine Your Spots
- Choose good lighting - natural daylight is best.
- Use a full‑length mirror and a hand‑held mirror to view hard‑to‑see areas (back, scalp, between toes).
- Gently stretch the skin and observe each spot for the criteria listed above.
- Take a close‑up photo with a ruler for scale; repeat the photo every 2‑3 months.
- Note any new symptoms like itching, tenderness, or bleeding.
If a spot changes in any way, schedule a check‑up.
When to Call a Dermatologist
A dermatologist is a medical doctor specialized in skin, hair, and nail health. Reach out when you notice:
- Any of the red‑flag features listed earlier.
- New spots appearing rapidly, especially after a recent sunburn.
- Persistent itching, pain, or oozing from a spot.
- Family history of melanoma or other skin cancers.
Dermatologists can perform a dermoscopic exam, biopsy suspicious lesions, and provide treatment options ranging from topical creams to surgical removal.
Quick Comparison: Benign Age Spot vs. Warning Sign
| Feature | Harmless Age Spot | Potential Warning Sign |
|---|---|---|
| Color | Uniform brown or tan | Variegated (brown, black, red, white, blue) |
| Border | Smooth, well‑defined | Irregular, scalloped, fuzzy |
| Shape | Symmetrical | Asymmetrical |
| Size | Usually < 6mm and stable | > 6mm or rapid growth |
| Texture | Flat, smooth | Raised, scaly, crusted, or bleeding |
Prevention Tips to Keep New Spots at Bay
- Apply broad‑spectrum SPF30+ sunscreen daily, even on cloudy days.
- Reapply sunscreen every two hours outdoors, or after swimming/sweating.
- Seek shade when the UV Index is 6 or higher (typically midday).
- Wear protective clothing: wide‑brimmed hats, long sleeves, UV‑blocking sunglasses.
- Avoid tanning beds - they emit intense UV radiation that accelerates pigment changes.
- Schedule an annual skin exam with a dermatologist, especially if you have a history of sunburns.

Frequently Asked Questions
Can age spots turn into skin cancer?
Most age spots are benign and stay that way. However, if a spot starts showing the red‑flag signs-especially rapid growth, new color, or irregular borders-it could be a precancerous lesion or early skin cancer. In those cases, a dermatologist’s evaluation is essential.
How often should I perform a self‑exam?
A quick visual check once a month is enough for most people. If you’re prone to sunburns or have a family history of skin cancer, consider a weekly review.
Is a dark mole the same as an age spot?
Not exactly. Moles (nevi) are clusters of pigment cells that can appear anywhere on the body, often from childhood. Age spots are flat patches that develop later in life due to sun exposure. Both can be brown, but their origins and risk profiles differ.
What does a dermatologist do during a skin check?
The doctor will use a dermatoscope-a magnifying lens with light-to examine lesions more closely. If a spot looks suspicious, they may perform a biopsy, removing a small tissue sample for lab analysis.
Can I treat age spots at home?
Over‑the‑counter brightening creams containing niacinamide, vitamin C, or hydroquinone can fade mild spots. For faster results, professional options like laser therapy or chemical peels are effective, but they should be done by qualified skin specialists.
Does sunscreen prevent existing age spots?
Sunscreen won’t erase spots that are already there, but it stops new ones from forming and can prevent existing spots from darkening further.
John and Maria Cristina Varano
October 3, 2025 AT 04:02These age spot tips are just basic US skin propaganda.
aarsha jayan
October 3, 2025 AT 16:00Hey everyone! 🌟 I love how this guide breaks down the scary stuff into bite‑size pieces. The color‑and‑border chart is super handy, especially for those of us who juggle busy lives and still want to keep an eye on our skin. I’d add that staying hydrated helps your skin’s natural repair mechanisms, so drink that water! Also, don’t forget to reapply sunscreen after swimming – the UV can sneak right back in. Keep spreading the knowledge and stay safe out there! 🌞
Maureen Crandall
October 3, 2025 AT 16:16Seriously you think the info is propaganda? It’s just science and common sense. No need to hype it.
Shivaraj Karigoudar
October 4, 2025 AT 00:20The physiological cascade that culminates in melanin deposition is fundamentally tied to ultraviolet photon absorption; when UVB photons strike keratinocytes, they trigger a signaling cascade that upregulates tyrosinase activity, which then catalyzes the conversion of tyrosine to dihydroxyphenylalanine and onward to eumelanin.
From a dermatological perspective, the UV index serves as a quantifiable metric of that photon flux, and values above 6 are considered sufficient to overwhelm the epidermal repair capacity.
Consequently, the skin responds by forming lentigines – colloquially known as age spots – as a protective barrier against further DNA damage.
Clinically, these lesions present as uniform brown macules with well demarcated borders, typically measuring less than six millimetres in diameter.
When you observe a deviation from this phenotype – such as variegated pigmentation, irregular borders, or an increase in size beyond the pencil‑eraser benchmark – the differential diagnoses expand to include actinic keratosis, lentigo maligna, or even early melanoma.
The ABCDE rule (asymmetry, border irregularity, colour variation, diameter >6 mm, evolution) remains the cornerstone of self‑assessment, albeit with the caveat that not all malignant lesions adhere strictly to these criteria.
It is also worth noting that cumulative photodamage can synergize with genetic predispositions, such as mutations in the CDKN2A gene, to accelerate oncogenic transformation.
Preventive strategies therefore hinge on both behavioural modifications – like diligent sunscreen application with SPF 30+ and re‑application every two hours – and periodic professional skin examinations, ideally biannually.
From a therapeutic standpoint, modalities such as cryotherapy, laser ablation, or topical retinoids can be employed to eradicate dysplastic lesions, but they require histopathologic confirmation before implementation.
Patients often underestimate the significance of subtle changes, assuming that a static spot will remain benign indefinitely; however, longitudinal monitoring with calibrated photographs can reveal insidious growth patterns that would otherwise be missed.
In addition, the psychosocial impact of visible age spots should not be trivialized, as they can affect self‑esteem and quality of life, prompting many individuals to seek cosmetic interventions.
Ultimately, the decision matrix balances oncologic risk, aesthetic concerns, and patient preferences, underscoring the importance of shared decision‑making in dermatologic care.
Remember, consistent sun protection not only curtails new spot formation but also mitigates the darkening of existing lesions, preserving skin integrity over the lifespan.
Should any of the red‑flag characteristics emerge – especially rapid enlargement, bleeding, or pruritus – a prompt dermatologic consultation is paramount to rule out malignancy.
Matt Miller
October 4, 2025 AT 11:26Great rundown – I’ll keep an eye on any changes and stay on top of sunscreen.
Fabio Max
October 4, 2025 AT 19:46I think the table does a solid job of breaking things down. It’s easy to spot the warning signs without needing a medical degree.
Darrell Wardsteele
October 4, 2025 AT 21:10While the guide is clear it could benefit from a stricter emphasis on regular dermatologist visits especially for those with a family history of skin cancer.
Madeline Leech
October 5, 2025 AT 09:40Honestly the whole “just keep an eye on them” spiel is nonsense – if you’re not checking your skin daily you’re basically inviting trouble. The US has some of the worst sun exposure rates and we can’t afford to be complacent.
Barry White Jr
October 5, 2025 AT 11:03Totally agree keep it simple apply sunscreen stay safe.
Andrea Rivarola
October 5, 2025 AT 23:33I’ve spent a lot of time reading up on dermal pigmentation and I must say that the interplay between UV‑induced DNA damage and melanocyte activity is both fascinating and a bit terrifying. When you consider that each sunburn can cause millions of pyrimidine dimers in the epidermal DNA, the cumulative effect over decades is substantial. Moreover, the epidermal turnover rate means that damaged cells are constantly being replaced, yet some mutated melanocytes can persist and expand, leading to the formation of lentigines. The clinical criteria you’ve outlined – color uniformity, border regularity, symmetric shape, size under six millimetres, and flat texture – are indeed the hallmarks of benign lesions. However, it is crucial to stress that any deviation from these parameters warrants a closer look, possibly with a dermatoscope, to evaluate pigment network patterns. In practice, I advise patients to maintain a skin diary, photographing lesions with a ruler for scale every few months. This longitudinal data can be invaluable when assessing subtle changes. Also, don’t underestimate the protective power of broad‑spectrum sunscreen; it not only prevents new spot formation but can also inhibit the darkening of existing macules. Lastly, while over‑the‑counter brightening creams can provide cosmetic improvement, they should never replace professional assessment, especially if any alarming signs appear.
Tristan Francis
October 6, 2025 AT 00:56Good info. Keep it short and simple.
Keelan Walker
October 6, 2025 AT 02:20Just wanted to say thanks for the detailed guide 😃 It really helps me stay on top of my skin health and I’ll definitely use the self‑exam steps you listed! 🌞👍
Heather Wilkinson
October 6, 2025 AT 03:43Happy to hear it’s useful! Keep monitoring and don’t hesitate to reach out if you need more tips 😊👩⚕️