Alcohol and Medications: Dangerous Interactions and Health Effects

Medication-Alcohol Interaction Checker
Check Your Medication Interactions
Enter your medications and get personalized guidance on alcohol safety. This tool helps you understand potential risks and makes informed decisions.
Select your medications and other factors to see interaction results.
More than 40% of adults in the U.S. take at least one medication that can react dangerously with alcohol. Many don’t even know it. You might think having a glass of wine with your painkiller or a beer after your antibiotic is harmless. But the truth? It’s not. These combinations aren’t just risky-they can kill.
How Alcohol Changes How Your Medications Work
Alcohol doesn’t just make you feel drunk. It changes how your body handles medicine. Two main things happen: your brain gets more depressed, and your liver gets overwhelmed. When you drink, alcohol slows down your central nervous system. That’s why you feel relaxed, sleepy, or uncoordinated. Many medications do the same thing-sleep aids, anxiety pills, painkillers. When you mix them, the effects multiply. It’s not 1 + 1 = 2. It’s more like 1 + 1 = 5. Your breathing can slow to dangerous levels. You might pass out. You might stop breathing entirely. At the same time, your liver is busy trying to break down both alcohol and your medication. They compete for the same enzymes. Sometimes, alcohol makes your body process the drug too slowly, so it builds up to toxic levels. Other times, it speeds things up, making the drug useless. Either way, you’re not getting the treatment you need-and you’re putting yourself at risk.Deadly Combos: Opioids, Benzodiazepines, and Alcohol
Some combinations are straight-up lethal. The CDC says 20% of opioid overdose deaths in 2020 involved alcohol. That’s not coincidence. It’s chemistry. Take oxycodone, hydrocodone, or methadone. These are powerful painkillers. Add alcohol, and your body absorbs them faster. With extended-release versions like OxyContin or Percocet, alcohol can trigger something called "dose-dumping." The drug releases all at once instead of slowly over hours. One study showed peak drug levels jumped two to six times higher when taken with alcohol. That’s not a bad reaction-it’s an overdose waiting to happen. Benzodiazepines like Xanax, Valium, or Ativan are even worse. A 2019 study found mixing them with alcohol increases overdose risk by 24 times. These drugs are meant to calm your nerves. Alcohol does the same. Together, they shut down your brain’s ability to control breathing. People don’t die from the painkiller. They die because they stop breathing. The FDA pulled a drug called Palladone off the market in 2005 after exactly this happened. Patients who drank while taking it overdosed-even when they took the right dose.Acetaminophen: The Silent Liver Killer
Tylenol is everywhere. Headache? Fever? Muscle soreness? You grab it without thinking. But if you drink, even moderately, you’re putting your liver in danger. Your liver breaks down acetaminophen into harmless waste-most of the time. But when alcohol is in the system, it shifts the process. Instead of safe byproducts, your liver starts making NAPQI, a toxic chemical. Normally, your body neutralizes it with glutathione. But alcohol depletes glutathione fast. Without it, NAPQI starts eating your liver cells. The FDA says acetaminophen overdoses-often tied to alcohol-cause 56,000 emergency room visits and 458 deaths every year in the U.S. You don’t need to binge drink. Just one drink with your nightly Tylenol can be enough, especially if you’ve been drinking regularly. Even if you don’t feel sick now, the damage builds. Chronic drinkers who take acetaminophen daily are at highest risk for sudden liver failure.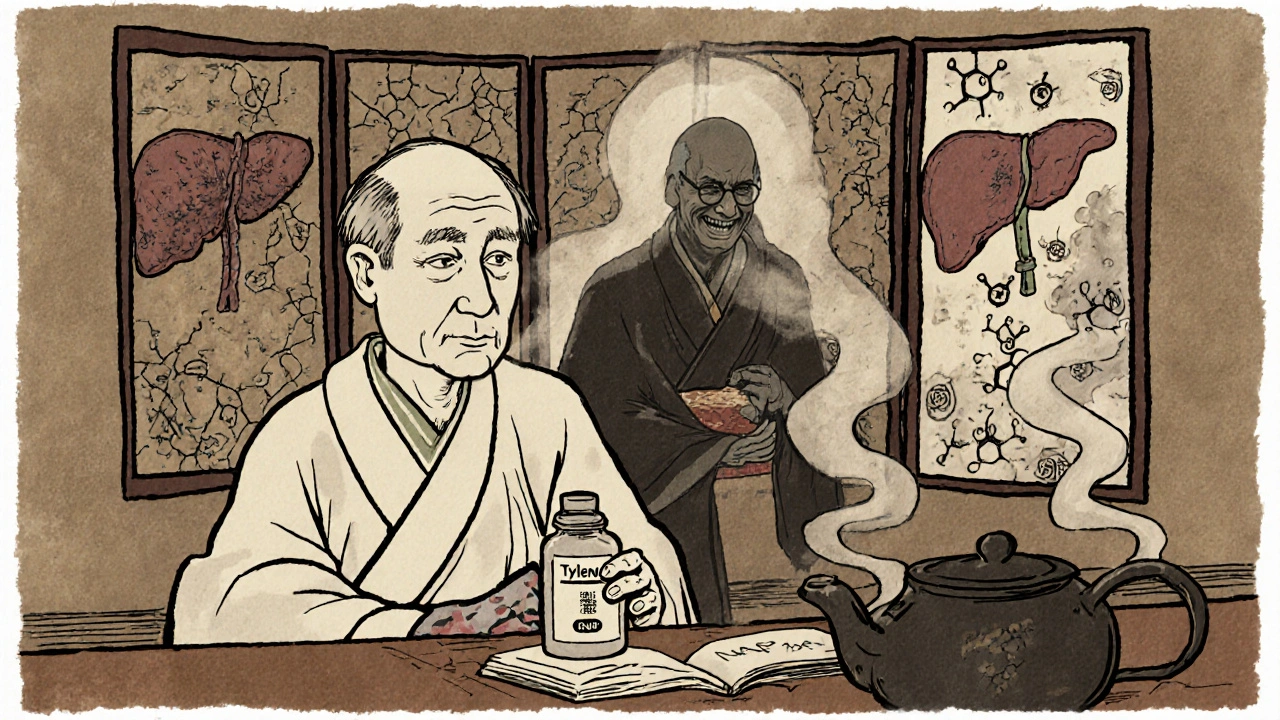
NSAIDs, Stomach Bleeding, and the Hidden Cost
Ibuprofen, naproxen, aspirin-these are common for pain and inflammation. You take them with food. You think you’re safe. But add alcohol, and you’re playing Russian roulette with your stomach. Both alcohol and NSAIDs irritate the stomach lining. Together, they wreck it. A 2017 meta-analysis found the risk of gastrointestinal bleeding triples to quintuples when you combine them. That’s not a stomach upset. That’s internal bleeding. You might feel fine until you pass out from blood loss. This isn’t just about heavy drinkers. Someone who has a glass of wine with dinner and takes Advil for back pain is at risk. Older adults are especially vulnerable because their stomach lining is thinner and heals slower.Antibiotics, Diabetes Meds, and Other Surprises
You might assume antibiotics are safe with alcohol. Not always. Metronidazole (Flagyl) causes a disulfiram-like reaction. Drink while taking it, and you’ll get nausea, vomiting, flushing, rapid heartbeat, and chest pain. It’s terrifying. The Illinois Poison Center says wait at least 72 hours after your last dose before drinking. Some antibiotics like linezolid and tinidazole have the same warning. Even azithromycin can make nausea and diarrhea worse. Diabetes meds are another hidden danger. Sulfonylureas like glipizide or glyburide can cause severe low blood sugar if you drink. Alcohol blocks the liver from releasing glucose. Combine that with a drug that forces your body to release insulin, and your blood sugar can crash to dangerous levels. The risk jumps 300%. You might pass out, have a seizure, or fall into a coma. Metformin, a common diabetes drug, carries a small risk of lactic acidosis when mixed with alcohol. It’s rare-but real. Limit yourself to one drink a day, if at all.
Who’s Most at Risk?
Not everyone is equally vulnerable. Some groups are walking into danger without knowing it. People over 65 are the most at-risk group. They take an average of 14 prescriptions a year. Their bodies process alcohol and drugs slower. Their liver and kidneys don’t work as well. They’re more likely to be on benzodiazepines, blood pressure meds, or painkillers-all high-risk for alcohol interactions. Women are at higher risk too. They have less body water, so alcohol concentrates faster in their blood. Even the same amount as a man will hit them harder. That means medication effects are stronger and last longer. Military veterans are another group. The VA found 30% of veteran suicides involved alcohol and prescription drugs. Many struggle with chronic pain, PTSD, and depression-leading to multiple medications and alcohol use. People with mental health conditions are 3.5 times more likely to have dangerous interactions. Depression, anxiety, bipolar disorder-they often come with prescriptions. Alcohol seems like a quick fix. But it makes symptoms worse and interferes with treatment.What You Should Do
You don’t have to give up alcohol forever. But you need to be smart. Read the label. The FDA requires warning labels on about 100 prescription drugs and 700 over-the-counter products. If it says "avoid alcohol," it’s not a suggestion. It’s a safety rule. Ask your pharmacist. They see your full medication list. They know what interacts. Don’t wait for them to warn you-ask. "Is it safe to drink while taking this?" Be honest with your doctor. If you drink, say so. Even if it’s just a glass of wine on weekends. They need to know to adjust your meds or warn you properly. Wait it out. If you’re on metronidazole, wait 72 hours. If you’re on a strong painkiller or sedative, skip alcohol entirely until you’re off it. If you’re on blood thinners or diabetes meds, avoid alcohol unless your doctor says it’s okay. Know the signs. If you feel unusually dizzy, confused, nauseous, short of breath, or have chest pain after drinking and taking medicine-get help immediately. Don’t wait.What’s Changing in Healthcare
Doctors and pharmacists are starting to catch up. The American Medical Association now requires physicians to screen for alcohol use when prescribing high-risk meds. Electronic health systems like Epic now block prescriptions if the patient has a history of alcohol use and is being given a dangerous combo. The FDA now requires new extended-release opioids to be tested for alcohol interactions before approval. Research is also moving toward genetic testing. Some people have a variant of the CYP2E1 enzyme that makes them 4.7 times more likely to suffer liver damage from acetaminophen and alcohol. Soon, we may be able to test for that risk before prescribing. But until then, the responsibility falls on you. No one else will check your bottle, your drink, and your meds every time.Can I have one drink with my prescription?
It depends on the medication. For some, like antibiotics or SSRIs, one drink might be okay-but only if your doctor says so. For others, like opioids, benzodiazepines, or metronidazole, even one drink can be deadly. Never assume it’s safe. Always check the label or ask your pharmacist.
Does alcohol make all medications less effective?
Not always. Sometimes alcohol makes medications stronger, which is more dangerous. Other times, it speeds up how fast your body breaks them down, making them less effective. For example, alcohol can reduce the effectiveness of antidepressants and make anxiety or depression worse. With blood pressure meds, it can cause your pressure to drop too low.
Is it safe to drink alcohol the night before taking medicine?
No. Alcohol stays in your system for hours, and its effects on liver enzymes can last days. If you drank the night before, your liver is still processing it. Taking acetaminophen, NSAIDs, or sedatives the next day can still trigger dangerous interactions. Wait at least 24-48 hours after your last drink before taking high-risk meds.
Why do older adults have more problems with alcohol and meds?
As we age, our liver and kidneys don’t work as well, so alcohol and drugs stay in the body longer. Older adults also take more medications-on average, 14 prescriptions a year. Many of those are for pain, sleep, or anxiety, which interact badly with alcohol. Plus, their bodies have less water, so alcohol hits harder. The Beers Criteria lists 30 medications that are especially risky for seniors when mixed with alcohol.
What should I do if I mixed alcohol and medication and feel sick?
If you feel dizzy, confused, nauseous, have trouble breathing, chest pain, or lose consciousness, call 911 or go to the ER immediately. Don’t wait. These symptoms can mean a life-threatening reaction. Even if you feel fine, call Poison Control at 1-800-222-1222 for advice. They’re available 24/7.
Bobby Marshall
November 1, 2025 AT 08:16Man, I never realized how many meds I was taking could turn a glass of wine into a one-way ticket to the ER. I’ve been popping Tylenol for headaches after work with a beer, thinking it’s harmless. Guess I’m lucky I haven’t ended up in the hospital. Time to read every label from now on. Thanks for laying this out like a gut-punch.
Cori Azbill
November 2, 2025 AT 16:15LOL. So now we’re blaming alcohol for everything? 🤡 Next thing you know, the FDA will ban bread because it ‘interacts’ with insulin. This is fear-mongering dressed up as public health. I’ve had whiskey with my oxycodone for years. Still breathing. Still working. Still not a zombie. 🍸💊
Carlo Sprouse
November 3, 2025 AT 23:10While I appreciate the clinical breakdown, this article lacks academic rigor. The CDC data cited is correlational, not causal. The 24x overdose risk for benzodiazepines + alcohol? That’s from a small retrospective cohort with confounding variables. The FDA’s withdrawal of Palladone was due to manufacturing issues, not pharmacokinetics. This is sensationalism masquerading as science. You’re not educating - you’re panic-selling.
Vinicha Yustisie Rani
November 4, 2025 AT 12:49In my village in India, people mix turmeric with whiskey for pain. No one dies. No one even gets sick. Maybe the problem isn't the alcohol - it's the pills. We used to trust our bodies. Now we trust labels. But bodies know more than any FDA warning. Maybe we should listen to them more.
Subham Das
November 4, 2025 AT 14:28It is, in essence, a metaphysical tragedy: we have outsourced our bodily sovereignty to pharmaceutical corporations and regulatory bureaucracies, only to then become terrified of the very substances that once granted us fleeting communion with the ineffable - wine, whiskey, the sacrament of the evening pour. We have forgotten that intoxication was once sacred, not a pharmacological error. Now, even the humble glass of Chardonnay is branded as a vector of death, a symbol of our collective failure to inhabit our flesh with dignity. The real poison is not ethanol - it is the institutionalized fear that has turned every sip into a sin.
And yet, the irony is not lost: the same system that vilifies alcohol is the one that profits from the very opioids and benzodiazepines it now deems lethal in tandem. Capitalism doesn’t care if you die - it only cares if you pay for the antidote.
So I ask you: when your doctor prescribes you 10 pills for a 3-day headache, who is truly responsible for the chemical ballet your liver must now perform? Is it you, the ignorant consumer? Or is it the system that commodifies suffering and then sells you the cure - while whispering, ‘Don’t drink.’
And yet, in the quiet of midnight, when the pills are swallowed and the glass is raised - isn’t it still the soul that seeks relief? Not the liver. Not the FDA. The soul.
Perhaps the real question isn’t whether alcohol interacts with your meds - but whether your life has become so devoid of meaning that you need both to numb the silence.
Ardith Franklin
November 4, 2025 AT 16:16Ever notice how every time a new study drops, Big Pharma quietly sponsors the journal? This whole ‘alcohol + meds = death’ narrative? It’s designed to push you toward their new ‘safe’ alternatives - which cost 10x more and have the same side effects. I’ve seen the data. The real killer is polypharmacy. Not wine. Not beer. The 14 pills your grandpa takes daily. And no one’s banning those. Funny, huh?
Deon Mangan
November 5, 2025 AT 00:13Wow. So you're telling me that if I take my Xanax and have a glass of wine... I might die? 😲 I mean, I knew it was bad, but I didn't realize it was like... *deadly* deadly. Like, ‘call 911 before you finish your glass’ deadly? 🤯 I’m gonna start keeping a journal: ‘Day 1: 1 wine + 1 Xanax - still alive!’ 🍷💊
Also, I think we should ban all meds. Just go back to herbs and prayer. And maybe yoga. And fasting. And drinking only moonwater. 🌙
Jenny Kohinski
November 5, 2025 AT 00:24This is such an important conversation. I’ve been on antidepressants for years and used to have a glass of wine every night to unwind. I didn’t realize it was making my anxiety worse - I thought I was just ‘relaxing.’ Now I’ve switched to herbal tea and it’s been life-changing. 🌿 Thank you for sharing this. You’re helping so many people - including me - feel less alone.
Aneesh M Joseph
November 5, 2025 AT 09:54So you’re saying don’t drink with meds? DUH. I thought that was common sense. Why is this even an article? My grandma knew that. She’d say, ‘Don’t mix your pills with the bottle.’ Simple. No science needed.
Cameron Daffin
November 6, 2025 AT 10:12Reading this made me pause. I’ve been taking ibuprofen for my back pain and having a beer after work like it’s nothing. I never thought about the bleeding risk - I just thought, ‘It’s just Advil.’ Now I’m gonna cut back. Maybe even switch to heat wraps. Honestly? This isn’t fear. It’s care. And I appreciate someone taking the time to lay it out like this. We’re all just trying to survive. Let’s not make it harder with hidden risks.
Also, I just bought a little pill organizer with labels. Small step, but I feel like I’m finally taking control. 🙏
Sharron Heath
November 7, 2025 AT 04:34While the medical information presented is largely accurate, the tone of this article risks alienating the very populations it aims to protect. The conflation of moderate consumption with abuse, coupled with alarmist language, may discourage individuals from seeking clarification from healthcare providers. A more balanced, evidence-based approach - emphasizing harm reduction rather than abstinence - would yield better public health outcomes.
Paul Orozco
November 8, 2025 AT 22:59My mother took her blood pressure meds and drank wine every night for 12 years. She’s 87. Still walks her dog. Still argues with the cable guy. Still makes the best lasagna in Ohio. So maybe, just maybe, your ‘dangerous interactions’ are just corporate scare tactics to sell more monitoring devices and expensive generic replacements. She didn’t read labels. She listened to her body. And it listened back.