Cervical Myelopathy: Recognizing Spinal Stenosis Symptoms and When Surgery Is Needed
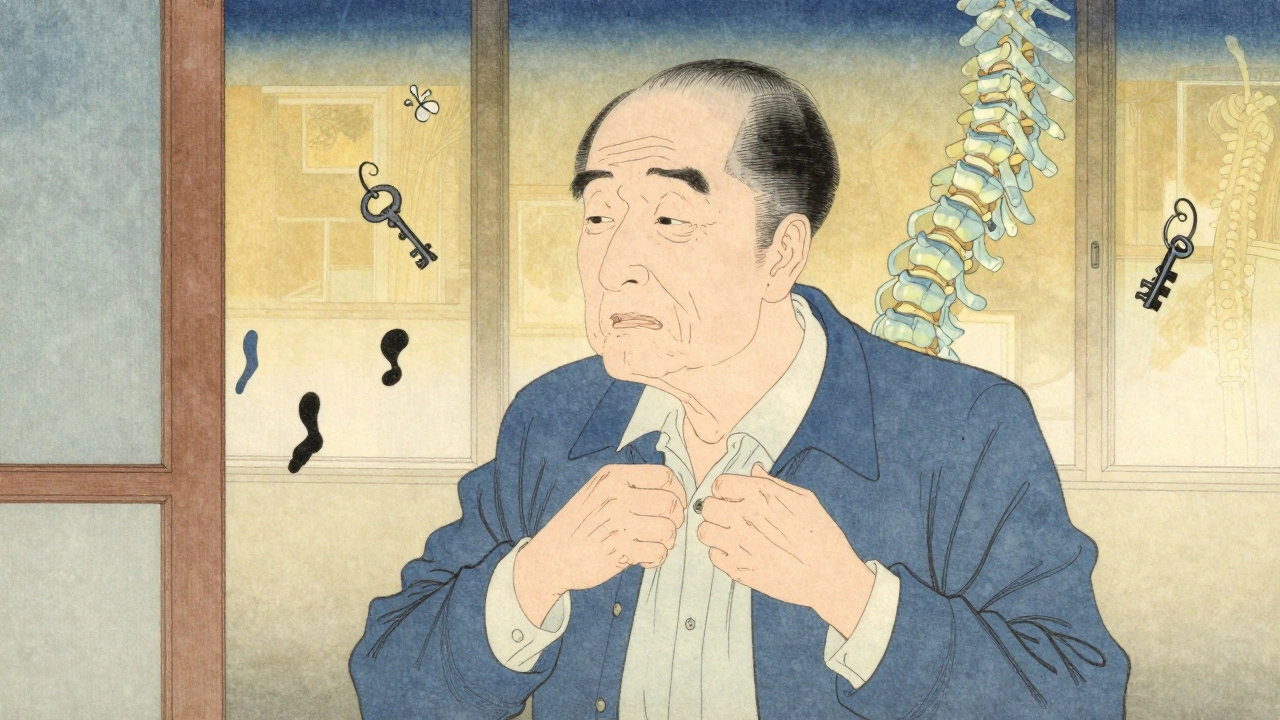
When your hands feel clumsy, your balance starts to slip, or you drop things you’ve held for years without trouble, it’s easy to blame aging. But these could be early signs of something more serious: cervical myelopathy. This isn’t just a stiff neck or a pinched nerve. It’s spinal cord damage caused by narrowing in your neck - a condition called cervical spinal stenosis. Left unchecked, it can lead to permanent weakness, loss of coordination, and even paralysis. The good news? If caught early, surgery can stop the damage - and in many cases, reverse it.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy isn’t just stenosis. It’s what happens when that narrowing actually hurts your spinal cord. Think of it this way: spinal stenosis is the pipe getting clogged. Cervical myelopathy is the water pressure bursting the pipe inside. The most common cause is cervical spondylotic myelopathy (CSM), which makes up about 75% of cases in people over 55. It’s not caused by trauma. It’s wear and tear - discs drying out, bones growing spurs, ligaments thickening - all slowly squeezing the spinal cord in your neck. The spinal canal in a healthy adult is about 17-18 millimeters wide. When it drops below 13 mm, it’s considered stenotic. At 10 mm or less, the cord is under serious pressure. That’s when symptoms start showing up. And they don’t come all at once. They creep in.Early Warning Signs You Can’t Ignore
Most people with cervical myelopathy don’t feel sharp pain. Instead, they notice things getting harder to do. The top early signs, reported in over 70% of patients, are:- Hand clumsiness - buttons won’t fasten, keys slip, writing gets messy
- Gait instability - feeling unsteady walking, as if your feet are stuck to the floor
- Balance problems - bumping into doorframes, tripping on flat surfaces
- Numbness or tingling in fingers or arms
- Stronger knee and ankle reflexes - something your doctor can spot during a simple exam
How Is It Diagnosed?
You can’t see this on an X-ray. A regular neck X-ray might show bone spurs or disc space narrowing - clues, but not proof. The gold standard is an MRI. It shows the spinal cord itself. If the cord has bright spots on T2-weighted images, that’s swelling or injury - clear evidence of myelopathy, not just stenosis. Doctors use the Japanese Orthopaedic Association (JOA) scale to measure severity. It scores movement, sensation, and bladder control out of 17. A score below 14 means you have myelopathy. A score under 12 usually means surgery is needed. Other tests like CT myelography or nerve conduction studies help confirm the diagnosis, especially if MRI isn’t possible. But the real bottleneck? Time. On average, people wait 14 months to get the right diagnosis. They see three or more doctors. By then, the cord may already be damaged beyond full recovery.Can You Treat It Without Surgery?
For a small group - about 28% - mild myelopathy (JOA 12-14) with no progression might stabilize with physical therapy, NSAIDs, and activity changes. But here’s the catch: 63% of those patients get worse over two years. That’s not a gamble worth taking. Physical therapy can help maintain strength and balance, but it won’t reverse cord compression. No pill, injection, or brace can undo the pressure on your spinal cord. That’s why experts agree: if your symptoms are moderate to severe, or if they’re getting worse, surgery isn’t optional - it’s the only way to prevent permanent disability.
When Surgery Is the Only Real Option
Surgery is recommended for JOA scores under 12, rapid progression, or signs of severe cord damage on MRI. Studies show 70-85% of patients improve after surgery - better hand function, steadier walking, fewer falls. There are two main surgical approaches:- Anterior (front): ACDF (removing the disc and fusing bones) or cervical disc replacement. Best for one or two levels. Success rate: 85-90% for neurological improvement.
- Posterior (back): Laminectomy or laminoplasty. Better for multi-level disease (three or more levels). Laminoplasty preserves motion and causes less post-op neck pain.
Timing Matters More Than You Think
This is the most critical point: the sooner you operate, the better you recover. Patients who have surgery within six months of symptom onset recover 37% better than those who wait over a year. Every month of delay reduces recovery potential by about 3%. That’s not a small number. It’s the difference between walking normally and needing a cane. One study found patients treated early were 2.7 times more likely to report “excellent” outcomes. Delayed surgery doesn’t just mean slower recovery - it means less recovery.What to Expect After Surgery
Hospital stays are short - one to two days for anterior surgery, two to three for posterior. Most people go home with a neck brace for a few weeks. Recovery takes 3-6 months. You’ll need formal physical therapy for 8-12 weeks. Focus isn’t on lifting weights - it’s on retraining your balance, coordination, and gait. Many patients need assistive devices like canes for months, even after successful surgery. Side effects vary:- ACDF: 22% have temporary trouble swallowing; 35% still have neck pain at six months
- Laminectomy: 18% develop chronic neck pain (“post-laminectomy syndrome”)
- Both: 5-7% risk of C5 nerve palsy (weak shoulder or arm), 1-2% risk of neurological worsening

Who Shouldn’t Have Surgery?
Not everyone is a candidate. People with severe heart or lung disease, uncontrolled diabetes (HbA1c over 7.0), or who smoke are at higher risk for complications. Smoking cuts fusion success by half. Quitting before surgery is non-negotiable. Also, if your MRI shows stenosis but no spinal cord signal changes - and you have no symptoms - you don’t need surgery. About 21% of people over 40 have stenosis without myelopathy. They’re fine. Monitoring is enough.The Bigger Picture
Cervical myelopathy is the most common cause of spinal cord problems in adults over 55. As the population ages, cases are rising. The cervical spine surgery market is expected to hit $3.4 billion by 2028. But here’s the warning: a 2023 study found 15-20% of current surgeries may be unnecessary. That’s why proper diagnosis is everything. You need MRI evidence of cord injury - not just stenosis - and clear neurological symptoms. New tools are emerging. Robotic-assisted surgery is getting more precise. Genetic markers like COL9A2 polymorphisms might one day tell us who’s at risk for faster degeneration. Clinical trials are testing drugs like riluzole to protect the cord during recovery. But for now, the best treatment is simple: recognize the signs early, get an MRI fast, and act before the damage becomes permanent.What to Do If You Suspect Cervical Myelopathy
If you’re experiencing hand clumsiness, balance issues, or unexplained weakness - especially if you’re over 55 - don’t wait. See a spine specialist. Ask for an MRI. Don’t settle for X-rays or physical therapy alone. If your symptoms are worsening, don’t delay. Surgery isn’t a last resort. It’s the best chance to keep your independence.Can cervical myelopathy get better without surgery?
In rare cases, mild cervical myelopathy may stabilize with conservative care, but only about 28% of patients improve over two years. Most - 63% - get worse. Surgery is the only proven way to stop progression and restore function in moderate to severe cases.
How do I know if I have cervical myelopathy and not just carpal tunnel?
Carpal tunnel causes numbness and tingling in the thumb, index, and middle fingers - usually worse at night. Cervical myelopathy affects the whole hand, causes weakness, clumsiness, and often includes balance problems, stiff legs, or urinary urgency. If you have symptoms in both hands plus gait issues, it’s likely spinal cord compression, not carpal tunnel.
Is cervical disc replacement better than fusion?
For single-level disease, disc replacement preserves motion and reduces future neck problems. Fusion is more predictable and has longer-term data. For multi-level disease, fusion or laminoplasty are usually preferred. The M6-C artificial disc is now approved for two or three levels and shows 81% success at two years, but it’s not for everyone. Your spine alignment and bone quality determine the best option.
How long does recovery take after cervical myelopathy surgery?
Most people go home in 1-3 days. Full recovery takes 3-6 months. Hand function often improves within 3 months, but gait and balance can take longer. Physical therapy for 8-12 weeks is critical. Some patients need canes or walkers for months, even after successful surgery.
Can I avoid surgery if my symptoms are mild?
If your JOA score is 12-14 and symptoms haven’t worsened in six months, your doctor may suggest monitoring with repeat MRIs and physical therapy. But if you notice any decline - even small things like dropping keys or stumbling - surgery should be discussed immediately. Waiting too long risks permanent damage.
Emily Haworth
December 12, 2025 AT 05:51Tom Zerkoff
December 14, 2025 AT 03:48Yatendra S
December 14, 2025 AT 06:40Himmat Singh
December 14, 2025 AT 16:34kevin moranga
December 14, 2025 AT 20:42