COPD Explained: Understanding Disease Stages and Effective Treatment Options
Chronic Obstructive Pulmonary Disease, or COPD, isn’t just a cough that won’t go away. It’s a serious, progressive lung condition that slowly steals your ability to breathe-especially when you least expect it. By 2023, over 380 million people worldwide were living with COPD, and it was the third leading cause of death globally. Most cases come from smoking, but long-term exposure to pollution, chemicals, or secondhand smoke can also trigger it. The good news? Even if you’ve been diagnosed, there are clear, proven ways to slow it down, manage symptoms, and live better. The key is knowing what stage you’re in-and what that actually means for your daily life.
What Are the Four Stages of COPD?
COPD doesn’t hit all at once. It creeps in, often ignored for years. Doctors use a simple breathing test called spirometry to measure how much air you can force out in one second-this is your FEV1. That number, compared to what’s normal for someone your age, height, and gender, tells you your stage.
Stage 1: Mild COPD - Your FEV1 is 80% or higher. You might notice a persistent morning cough with phlegm, or get winded after climbing stairs. But most people brush it off as aging or being out of shape. In fact, nearly half of people with Stage 1 COPD don’t even know they have it. That’s dangerous. At this point, quitting smoking can cut disease progression by up to 50%.
Stage 2: Moderate COPD - FEV1 drops to 50-79%. Now the shortness of breath is harder to ignore. Walking across a room or doing light housework leaves you gasping. You might find yourself stopping every few minutes just to catch your breath. This is when most people finally see a doctor. Spirometry confirms it, and treatment begins-not just to feel better, but to prevent faster decline.
Stage 3: Severe COPD - FEV1 falls to 30-49%. Breathing becomes a constant effort. Getting dressed, cooking a meal, or showering can leave you exhausted. Exacerbations-sudden worsening of symptoms-are frequent, often requiring emergency care or steroids. Oxygen levels may dip below 88% during activity. At this stage, your lungs are significantly damaged, but there’s still time to improve quality of life with the right plan.
Stage 4: Very Severe (End-Stage) COPD - FEV1 is below 30%, or under 50% with chronic low oxygen. Breathing is hard even at rest. Many need oxygen 24/7. Simple tasks like brushing teeth or talking on the phone become exhausting. Some develop cyanosis-a bluish tint to lips or fingertips-from lack of oxygen. This stage carries high risk of heart problems, lung infections, and sudden, life-threatening flare-ups. Survival improves with continuous oxygen therapy, but the focus shifts from slowing disease to managing comfort and avoiding hospitalizations.
How Treatment Changes With Each Stage
Treatment isn’t one-size-fits-all. It evolves with your lung function and symptoms. The goal? Reduce breathlessness, prevent flare-ups, and keep you moving as long as possible.
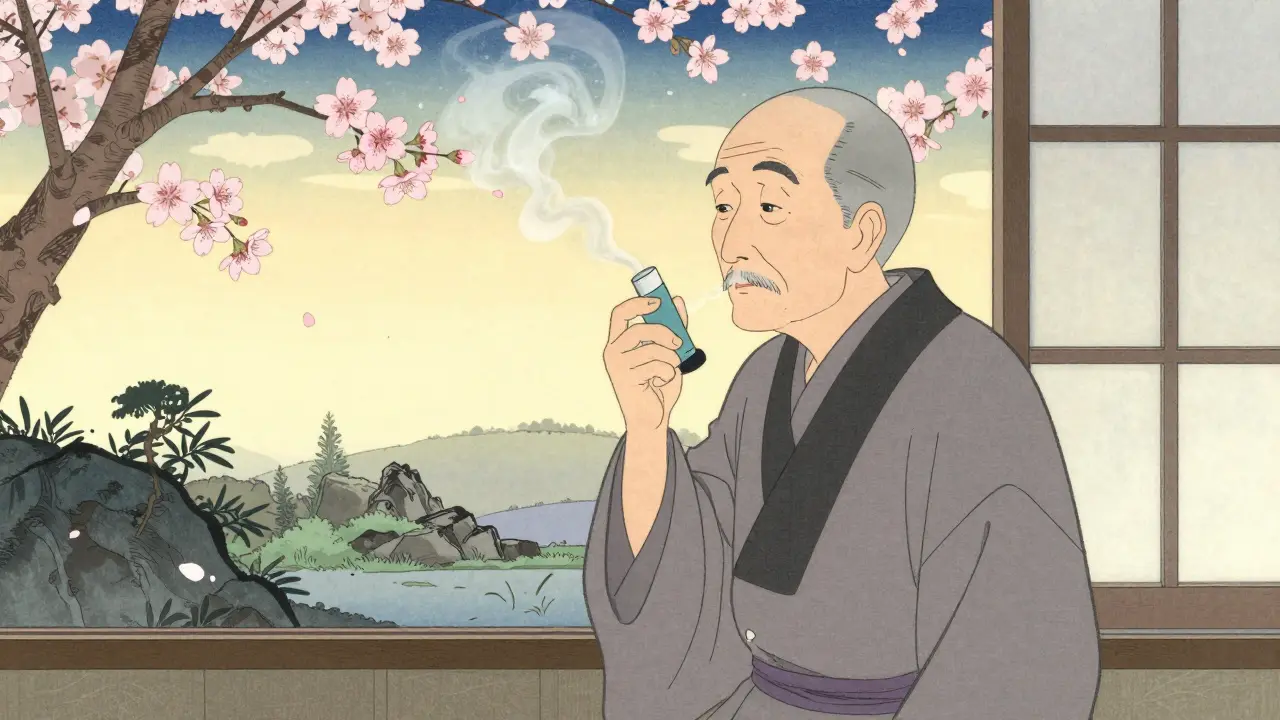
At Stage 1, the most powerful tool is quitting smoking. Nothing else comes close. Short-acting inhalers like albuterol are used only when needed-for sudden breathlessness. No daily meds yet. Just lifestyle changes and education.
Stage 2 usually means adding long-acting inhalers: either tiotropium (Spiriva) or salmeterol (Serevent). These keep airways open for 12-24 hours. Pulmonary rehab becomes critical. It’s not just exercise-it’s breathing techniques, nutrition advice, and mental support. Studies show people who complete rehab can walk 54 meters farther in six minutes. Annual flu shots and pneumococcal vaccines are non-negotiable.
Stage 3 often requires combination therapy: a long-acting beta-agonist (LABA) plus a long-acting muscarinic antagonist (LAMA). If you’ve had two or more flare-ups in a year, your doctor may add an inhaled steroid. Oxygen therapy starts if your blood oxygen drops below 88% during activity. At this point, daily routines change. You might need help with chores, or avoid crowded places where infections spread easily.
Stage 4 demands aggressive, continuous care. Oxygen therapy for 15+ hours a day can extend life by 44% in those with severe low oxygen. Portable oxygen units help, but they’re bulky and last only 4-6 hours on a full charge. For some, lung volume reduction surgery-removing damaged parts of the lung-can improve breathing and survival. Lung transplant is an option for those under 65 with FEV1 under 20%, but it’s rare and requires a long waitlist. Palliative care becomes part of the plan, focusing on comfort, not cure.
What Works Beyond Medication
Medicines help, but they’re only half the story. The real game-changers are habits and support systems.
Pulmonary rehabilitation isn’t optional-it’s essential. Programs last 8-12 weeks, with two sessions a week. You’ll learn how to breathe efficiently, strengthen your diaphragm, and manage anxiety. Studies show it cuts hospital visits by 37%. And it’s covered by Medicare if you meet criteria: confirmed COPD, FEV1 under 55%, and documented symptoms.
Nutrition matters more than people think. Many with advanced COPD lose weight because breathing burns so many calories. A dietitian can help you eat enough protein and calories without bloating-which makes breathing harder. Avoiding sugary drinks and processed foods helps reduce mucus.
Vaccines are your shield. Flu season? Get the shot. Pneumonia? Get the pneumococcal vaccine. COVID-19? Stay up to date. One infection can send you to the hospital for weeks.
And don’t underestimate emotional health. Anxiety and depression are common. One Reddit user wrote, “I stopped leaving the house because I was scared I’d collapse.” Therapy, support groups, or even just talking to someone who gets it makes a huge difference. The COPD Foundation runs over 85 local support groups and a 25,000-member online community.

The Hidden Struggles No One Talks About
COPD isn’t just about lungs. It’s about money, mobility, and dignity.
Spiriva costs $350-$400 a month without insurance. Many patients skip doses because they can’t afford it. Oxygen equipment is bulky, noisy, and limits travel. Most portable units only last half a day. Medicare covers 80% after a $233 deductible, but the rest adds up.
Using inhalers correctly? Harder than it looks. Studies show 70-80% of patients use them wrong-pressing too early, not holding breath long enough. That means less medicine reaches the lungs. Most need 3-5 supervised sessions to get it right.
And then there’s the loneliness. One Stage 4 patient shared: “I can’t shower without oxygen. Brushing my teeth leaves me gasping.” Daily life becomes a series of small defeats. That’s why self-management tools-like the FDA-cleared Kyna COPD app, which predicts flare-ups with 82% accuracy-are gaining ground. But adoption is low. Only 28% of patients use them, even though they cut exacerbations by 22%.
What’s New in COPD Treatment?
The field is evolving fast. In September 2023, the FDA approved Breztri Aerosphere, the first single-inhaler triple therapy for COPD and asthma-COPD overlap. It combines three drugs in one device, simplifying treatment for complex cases.
Another promising drug, ensifentrine, is a new type of bronchodilator. In late-stage trials, it improved FEV1 by 13%-better than some existing options. It’s expected to be available by 2027.
Genetics is also stepping in. The NIH’s COPDGene study found 82 genetic variants linked to how fast COPD progresses. This could lead to personalized treatments-matching drugs to your DNA.
Telehealth adoption has exploded. In 2020, only 15% of pulmonologists used virtual visits. By 2023, it was 62%. Many now offer hybrid care: in-person checkups combined with remote symptom tracking. This is especially helpful for those in rural areas or with limited mobility.

What You Can Do Right Now
If you’re worried about COPD-whether you smoke, have a chronic cough, or get winded easily-get tested. Spirometry takes five minutes. It’s cheap, painless, and life-changing.
If you’ve been diagnosed:
- Quit smoking-today. Even after years, your lungs will heal some.
- Ask for pulmonary rehab. Don’t wait until you’re in Stage 3.
- Learn your inhaler technique. Ask your pharmacist to watch you use it.
- Get vaccinated every year-flu, pneumonia, COVID-19.
- Join a support group. You’re not alone.
- Track your symptoms. Use a notebook or app. Notice what triggers breathlessness.
COPD is not a death sentence. It’s a condition you can manage-with the right knowledge, tools, and support. The earlier you act, the more life you’ll have left to live well.
Can COPD be reversed?
No, COPD cannot be reversed. Damaged lung tissue doesn’t heal. But its progression can be slowed significantly-especially if you quit smoking early. Medications, pulmonary rehab, and oxygen therapy can help you maintain function and avoid flare-ups, so you live longer and feel better.
Is COPD the same as asthma?
No. Asthma is usually reversible with medication and often starts in childhood. COPD is progressive, usually caused by long-term smoke exposure, and typically appears after age 40. Some people have both-called asthma-COPD overlap syndrome (ACOS)-which requires different treatment.
How do I know if I’m having a COPD flare-up?
Signs include worsening shortness of breath, more coughing, thicker or colored mucus (yellow, green, or bloody), increased use of rescue inhalers, swelling in ankles, or feeling more tired than usual. If you notice these, contact your doctor immediately. Early treatment can prevent a hospital stay.
Can I still travel with COPD?
Yes, but planning is key. Talk to your doctor before flying-airplane cabins have lower oxygen levels. Bring extra oxygen, a copy of your prescription, and a letter from your provider. Portable oxygen concentrators are allowed on planes, but you must notify the airline 48 hours in advance. Avoid high altitudes and extreme temperatures.
What’s the life expectancy with COPD?
It varies widely. Someone with Stage 1 COPD who quits smoking may live a normal lifespan. Stage 4 patients with chronic low oxygen have a higher risk of early death, but continuous oxygen therapy can add years. Many factors matter: age, smoking status, comorbidities like heart disease, and how well you follow your treatment plan. Focus on managing your health-not just the numbers.
Why do I feel more breathless in cold weather?
Cold air causes your airways to tighten, making breathing harder. Dry air also irritates lungs. In winter, wear a scarf over your nose and mouth to warm and humidify the air before it enters your lungs. Stay indoors on very cold or smoggy days. Use a humidifier at home.
Are there any new drugs coming for COPD?
Yes. Ensifentrine, a new type of bronchodilator, showed strong results in 2023 trials and could be available by 2027. Researchers are also testing gene therapies and anti-inflammatory drugs targeting specific COPD subtypes. The goal is to move from one-size-fits-all to treatments tailored to your lung damage pattern and genetics.
Next Steps If You’re Living With COPD
Start with one thing: schedule a spirometry test if you haven’t had one. If you already know your stage, review your treatment plan with your doctor. Ask: “Am I on the right meds? Do I need rehab? Should I be on oxygen?”
If you’re a caregiver, learn how to help with inhaler technique, recognize flare-up signs, and support emotional health. Don’t wait for a crisis. Prevention is everything.
COPD is a marathon, not a sprint. Progress isn’t always measured in lung numbers-it’s in how many stairs you can climb, how many meals you can cook, how many days you can spend with family without feeling wiped out. Every small step counts.
John O'Brien
January 27, 2026 AT 18:07Kegan Powell
January 29, 2026 AT 09:46astrid cook
January 29, 2026 AT 20:52Andrew Clausen
January 30, 2026 AT 21:28Anjula Jyala
January 31, 2026 AT 17:51Kirstin Santiago
February 1, 2026 AT 12:30Conor Flannelly
February 2, 2026 AT 22:36Conor Murphy
February 3, 2026 AT 21:59