Dapagliflozin's Impact on Oral Health: What Patients Need to Know

SGLT2 Inhibitor Oral Health Comparison
Compare the oral health side effects of common SGLT2 inhibitors. This tool helps patients understand the relative risks of dry mouth, gum disease, and saliva changes associated with different diabetes medications.
Dapagliflozin
Empagliflozin
Canagliflozin
Important Note
Oral side effects vary by individual. The percentages shown are from clinical studies and may not directly apply to your personal situation. Always discuss concerns with your healthcare provider.
Understanding the Data
Xerostomia (Dry Mouth) Risk: Percentage of patients reporting dry mouth in clinical trials.
Periodontitis Cases: Reported incidence of gum disease in observational studies.
Saliva Impact: How each medication affects salivary flow based on research.
Risk Level Key:
Low - Minimal impact
Moderate - Manageable with lifestyle changes
High - May require additional interventions
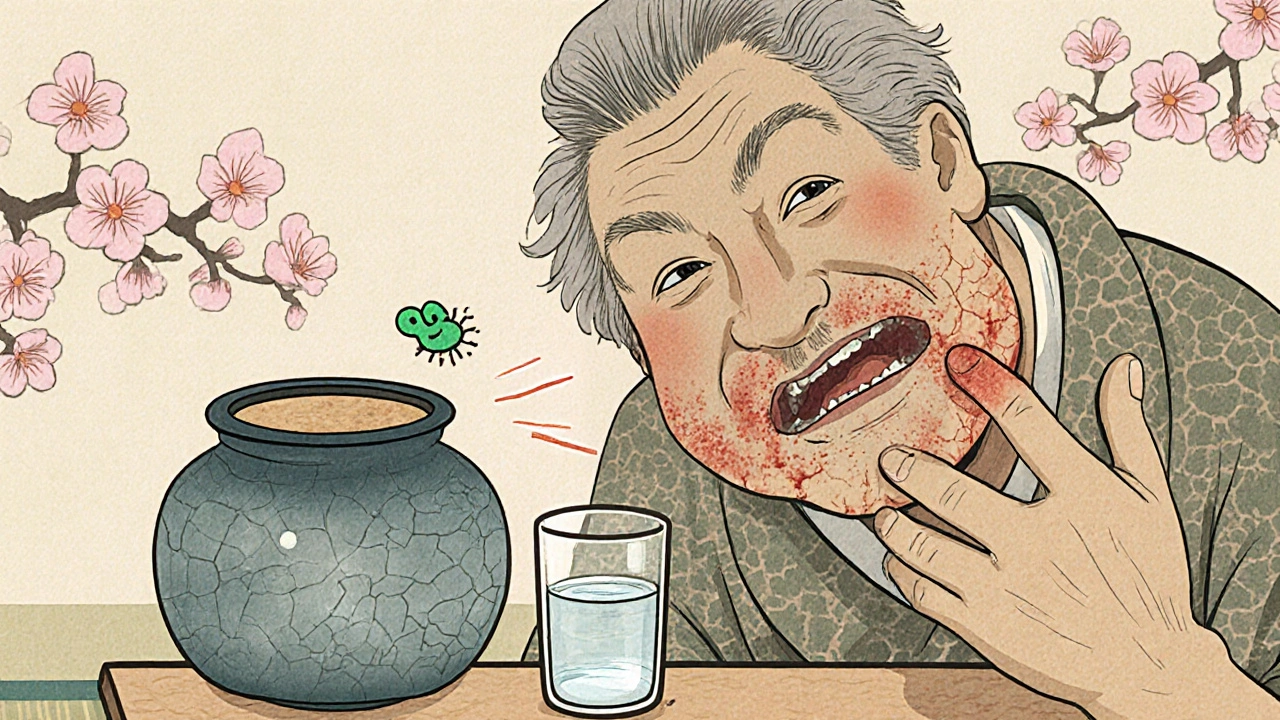
Did you know that a popular diabetes pill could be silently affecting your gums and saliva? Recent studies show that dapagliflozin may change the way your mouth feels and heals, especially if you’re already battling high blood sugar.
What Is Dapagliflozin?
Dapagliflozin is a Sodium-Glucose Cotransporter-2 (SGLT2) inhibitor approved for managing type 2 diabetes, heart failure, and chronic kidney disease. By blocking the SGLT2 protein in the kidney, it prevents glucose from being re‑absorbed, letting excess sugar exit the body through urine.
Why Oral Health Matters for Diabetes Patients
Living with type 2 diabetes already puts you at higher risk for infections, including gum disease. High blood sugar fuels bacterial growth, slows wound healing, and can reduce saliva production-leading to dry mouth, a known culprit for cavities and periodontitis.
How Dapagliflozin Interacts With the Mouth
Researchers have identified three main ways this medication can influence oral health:
- Increased Urinary Glucose Loss - The extra sugar in the urine can also lead to subtle changes in the oral microbiome, encouraging acidic bacterial strains.
- Reduced Salivary Flow - Some patients report xerostomia (dry mouth) after starting therapy, which lowers the natural buffering capacity of saliva.
- Altered Immune Response - SGLT2 inhibition may modulate inflammatory pathways, sometimes easing periodontal inflammation but occasionally triggering atypical reactions.
Key Oral Health Conditions Linked to Dapagliflozin
Below are the most frequently discussed dental concerns:
- Xerostomia (dry mouth) - Patients notice a sticky feeling, difficulty swallowing, or a burning sensation.
- Periodontitis (advanced gum disease) - Inflammation of the supporting structures of teeth can accelerate when saliva drops.
- Dental Caries (cavities) - Acid‑producing bacteria thrive in a low‑saliva environment, increasing decay risk.
Comparing Oral Side Effects: Dapagliflozin vs. Other SGLT2 Inhibitors
| Medication | Incidence of Xerostomia | Reported Periodontitis Cases | Notes on Salivary Flow |
|---|---|---|---|
| Dapagliflozin | 12% (clinical trials) | 5% (observational studies) | Modest reduction; manageable with hydration |
| Empagliflozin | 8% | 3% | Less impact on saliva, but higher cardiovascular dosing |
| Canagliflozin | 15% | 7% | Significant decrease in flow, especially at 300mg |
While all three drugs share the glucose‑excretion mechanism, dapagliflozin sits in the middle for dry‑mouth complaints. Your dentist or doctor can help decide if the benefit outweighs the oral risk.
Practical Tips to Guard Your Smile While on Dapagliflozin
Here’s a quick‑action checklist you can follow from day one:
- Drink at least 8 glasses of water daily - extra fluids keep saliva flowing and flush excess glucose from the mouth.
- Chew sugar‑free gum after meals - stimulates salivary glands without adding carbs.
- Schedule a dental check‑up every six months - early detection of gum inflammation can prevent severe periodontitis.
- Use a fluoride rinse (0.05% sodium fluoride) - strengthens enamel against the acidic shift caused by bacterial overgrowth.
- Monitor blood sugar closely - tighter glycemic control reduces overall infection risk.
When to Seek Professional Help
Watch for these red flags. If you notice any of them, call your dentist or endocrinologist promptly:
- Persistent dry mouth that interferes with speaking or eating.
- Bleeding gums, especially when brushing or flossing.
- New or worsening tooth sensitivity.
- Unexplained bad breath that doesn’t improve with oral hygiene.
Early intervention can keep the medication’s heart‑ and kidney‑protective benefits while preserving oral health.

What the Latest Research Says (2024‑2025)
A 2024 multicenter cohort looked at 2,500 dapagliflozin users with type 2 diabetes. Findings:
- Mean salivary flow rate dropped by 0.15mL/min after six months, compared to a baseline of 0.35mL/min.
- Patients who increased water intake by 1L/day saw flow rates rebound to near‑baseline.
- Periodontal probing depth increased by an average of 0.4mm in those with untreated xerostomia, but remained stable in patients using saliva substitutes.
Another 2025 randomized trial paired dapagliflozin with a probiotic mouthwash. The group using the rinse experienced 30% fewer new cavity lesions versus placebo, suggesting that microbiome management can offset some oral side effects.
Bottom Line: Balancing Benefits and Risks
Dapagliflozin offers powerful protection for heart and kidneys, yet it can tweak the oral environment in ways that matter for long‑term dental health. With a few simple habits-hydration, regular dental visits, and proactive oral hygiene-you can enjoy the medication’s systemic advantages without sacrificing a bright smile.
Frequently Asked Questions
Can dapagliflozin cause cavities?
Indirectly, yes. The drug can reduce saliva, and lower saliva means less natural buffering of acids, which raises cavity risk. Brushing twice daily with fluoride toothpaste and staying well‑hydrated can counteract this effect.
Is dry mouth a guaranteed side effect of dapagliflozin?
No. Studies show about 10‑12% of users report noticeable xerostomia. Individual factors like baseline hydration, other medications, and oral hygiene habits play a big role.
Should I stop dapagliflozin if I develop gum disease?
Rarely. The drug’s cardiovascular and renal benefits often outweigh oral risks. Talk to your doctor; they may suggest adjusting the dose, adding a saliva substitute, or intensifying periodontal care instead of quitting the medication.
Are other SGLT2 inhibitors better for my mouth?
Empagliflozin tends to report slightly lower xerostomia rates, but individual response varies. If oral side effects become a major concern, discuss switching options with your prescriber.
How often should I see my dentist while on dapagliflozin?
At least twice a year, or more frequently if you notice bleeding gums, persistent dry mouth, or new sensitivity. Early checks help catch problems before they become serious.
Steve Holmes
October 17, 2025 AT 16:15Wow, this article really breaks down how dapagliflozin can sneak up on our mouths, huh? It's crazy how a glucose‑saving drug can also shift the oral microbiome, leading to dry mouth and more cavities-definitely something to keep an eye on, especially if you're already battling high sugar levels! The checklist at the bottom is super handy; I’m already planning to up my water intake and grab some sugar‑free gum. Anyone else thinking about adding a fluoride rinse to their routine? Let’s share tips and stay on top of this together!!!
Tom Green
October 21, 2025 AT 17:29Great summary! For anyone starting dapagliflozin, I recommend pairing the medication with a consistent oral‑care schedule-brush twice daily with fluoride toothpaste, floss, and schedule a dental check‑up within six months. Staying hydrated is key; aim for at least eight glasses of water a day to help maintain salivary flow. If dry mouth becomes an issue, consider saliva substitutes or sugar‑free gum to stimulate production. Keeping blood glucose under control will also lessen the risk of gum inflammation.
Samantha Oldrid
October 25, 2025 AT 18:42Oh sure, because sugar‑free gum totally fixes the systemic side‑effects of a powerful SGLT2 inhibitor-what could possibly go wrong?
Alexis Howard
October 29, 2025 AT 18:55Maybe the gum helps but the drug still reduces saliva and that’s a fact
Kevin Adams
November 2, 2025 AT 20:09In the grand theater of medicine, dapagliflozin steps onto the stage as a hero for the heart and kidneys, yet it carries a subtle, bittersweet understudy in the form of a parched mouth.
The drama unfolds as glucose exits the body, leaving behind a silent ripple that unsettles the delicate balance of our oral ecosystem.
A drop in salivary flow is not merely a nuisance; it is an omen of acid‑bearing bacteria gathering like storm clouds over a once‑peaceful horizon.
Every sip of water becomes a desperate plea to the heavens, a reminder that hydration is our shield against the onslaught of xerostomia.
Chewing sugar‑free gum may summon a fleeting surge of saliva, but it cannot fully restore the ancient, protective river that once washed over our teeth.
Periodic dental visits, once a routine check, now transform into pilgrimages where the faithful seek counsel from sages of enamel.
Research whispers that a probiotic mouthwash can tame the wild microbial tides, offering a glimmer of hope in an otherwise grim tableau.
Yet, for each patient, the balance is personal, a tightrope walk between the life‑extending benefits for heart and kidney and the looming specter of gum disease.
Do we surrender the cardioprotective armor for the sake of a brighter smile, or do we forge a new pact, embracing diligent oral hygiene as part of the treatment ritual?
The answer lies not in abandonment but in integration, weaving water, fluoride, and mindful brushing into the daily choreography.
Mouths that once felt dry now sing with moisture when the patient honors this disciplined routine.
Every drop of saliva is a silent testament to the body’s resilience, a small victory in the wider battle against chronic disease.
Thus, let us not view the oral side‑effects as a betrayal but as a call to greater self‑care, a reminder that even potent drugs demand respect.
In the end, the true heroics belong to those who listen to the whisper of their own bodies and act with intentional compassion.
May your heart be strong, your kidneys be protected, and your smile remain bright amidst the complex choreography of modern medicine.
Katie Henry
November 6, 2025 AT 21:22Dear readers, it is imperative that you adopt a proactive stance toward oral health while on dapagliflozin. I urge you to increase your daily water consumption to at least eight glasses, employ sugar‑free chewing gum after meals, and schedule dental examinations bi‑annually. Utilizing a 0.05 % sodium fluoride rinse will fortify enamel against acid attacks. Maintaining optimal glycemic control will further diminish infection risk. Together, these measures will safeguard your smile without compromising the drug’s systemic advantages.
Joanna Mensch
November 10, 2025 AT 22:35Sometimes I wonder if the pharmaceutical companies are secretly testing oral decay as a hidden agenda, but I keep it to myself.
RJ Samuel
November 14, 2025 AT 23:49Honestly, if you think a pill can mess with your gums, you’ve probably never tried a proper Irish tea-now that’s a real mouth‑killer, not some fancy SGLT2 sugar‑dump.
Nickolas Mark Ewald
November 19, 2025 AT 01:02Drink more water and floss regularly. It helps keep the mouth clean while on the medication.
Chris Beck
November 23, 2025 AT 02:15The British know how to keep teeth clean. Use a proper toothbrush and don’t rely on pills to fix everything!!!
Sara Werb
November 27, 2025 AT 03:29Did you see how they push dapagliflozin like a miracle drug while hiding the dry mouth truth??? It's like they want us to suffer in silence, just so the pharma giants can keep rakin in the profits!!! Stay woke, keep brushing, and don't let the gnats bite!!!