Dry Eyes from Medications: Lubrication and Lifestyle Tips to Manage Side Effects

Medication Dry Eye Risk Calculator
Dry Eye Risk Assessment
Enter the medications you're currently taking to assess your risk of medication-induced dry eyes.
How It Works
Dry eyes from medications are common. This tool assesses your risk based on the medications you're taking.
- Antihistamines Medium Risk
- Antidepressants Medium Risk
- Blood Pressure Meds Medium Risk
- Glaucoma Drops (BAK) High Risk
- Isotretinoin High Risk
Risk Assessment Results
Enter medications to see your risk assessment
More than 1 in 4 people with dry eyes aren’t dealing with age or screen time-they’re dealing with their prescriptions. If you’ve been reaching for eye drops more often lately, and you’ve started taking a new medication, it might not be coincidence. Dry eyes from medications is a real, widespread issue, and it’s often overlooked. You’re not imagining it. Your eyes really do feel gritty, burning, or tired after taking certain pills, even if you’ve been careful about screen use or dry air.
Which Medications Cause Dry Eyes?
It’s not just one drug. Dozens of common prescriptions can mess with your tear system. Some block the signals your body uses to make tears. Others dry you out internally, or damage the oily layer that keeps tears from evaporating too fast. The worst offenders include:
- Antihistamines like Benadryl, Claritin, and Zyrtec-these are designed to reduce allergies, but they also shut down tear production.
- Antidepressants such as Zoloft, Prozac, amitriptyline, and nortriptyline-these affect brain chemicals, but they also quiet down the nerves that tell your eyes to produce tears.
- Blood pressure meds like metoprolol, atenolol, and diuretics (Lasix, hydrochlorothiazide)-these lower fluid in your body, and your eyes are one of the first places to feel it.
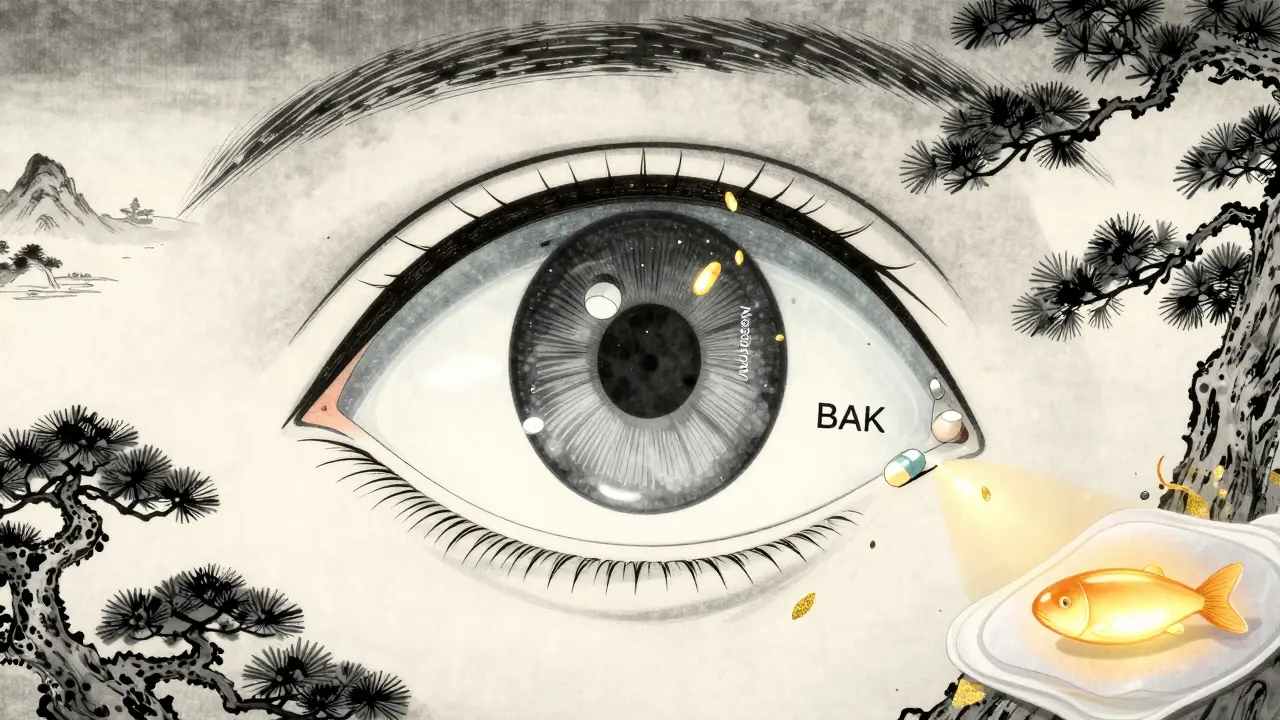
- Glaucoma eye drops-yes, the very drops meant to protect your vision can cause dryness. Why? Many contain benzalkonium chloride (BAK), a preservative that’s toxic to the eye surface over time. Up to 47% of users report stinging and dryness, but switching to preservative-free versions cuts that in half.
- Isotretinoin (Accutane)-this powerful acne treatment can permanently shrink oil glands in your eyelids, leading to chronic tear evaporation.
- Chemotherapy drugs like methotrexate and cisplatin-these attack fast-growing cells, including those in your tear glands.
Even newer drugs-like immune checkpoint inhibitors for cancer or DPP-4 inhibitors for diabetes-are showing up in studies as culprits. The more meds you take, the higher your risk. For people over 65 on five or more prescriptions, up to 40% experience medication-induced dry eye.
How Your Eyes Get Damaged
Your tears aren’t just water. They’re a three-layer system: mucus to stick to the eye, water to hydrate, and oil to seal it in. Medications can break any part of this.
- Anticholinergic drugs (like antihistamines and some antidepressants) block the nervous system signals that tell your lacrimal gland to make tears. Less tear production = dry surface.
- Diuretics pull water from your whole body, including your eyes. Your tear volume drops because your body thinks it’s dehydrated.
- Isotretinoin and some glaucoma drops clog or destroy your meibomian glands-the tiny oil glands in your eyelids. Without that oil layer, tears evaporate in seconds.
- Preservatives like BAK in eye drops don’t just kill bacteria-they also damage the surface cells of your eye. Over time, this makes your eyes more sensitive and less able to heal.
This isn’t just discomfort. Left untreated, chronic dryness can lead to corneal scratches, infections, and even vision changes. That’s why managing it isn’t optional-it’s necessary.
Lubrication That Actually Works
Not all eye drops are created equal. If you’re using preserved artificial tears more than four times a day, you might be making things worse. The preservatives add up. Instead, go for preservative-free options.
- Preservative-free artificial tears-use them 4 to 6 times a day. Brands like Systane Ultra PF, Refresh Optive PF, or Thealoz Duo are designed for daily use without irritation. They’re slightly more expensive, but your eyes will thank you.
- Timing matters-if you’re on glaucoma drops, wait 15 minutes after your prescription drop before using your artificial tear. That way, the medication doesn’t get washed out.
- Application technique-tilt your head back, gently pull down your lower lid, and let the drop fall into the pocket. Don’t let the bottle touch your eye. One study found this simple change improved effectiveness by 25%.
For stubborn cases, doctors may prescribe:
- Cyclosporine (Restasis, Cequa)-this reduces inflammation and helps your body make more tears. It takes 3 to 6 months to work, but users report 15-20% more tear production. Cequa’s new nanomicellar formula works 300% better than older versions.
- Lifitegrast (Xiidra)-this targets inflammation directly and reduces symptoms by 30% in clinical trials. Many users feel relief within 2 weeks.
- Punctal plugs-tiny, painless devices inserted into tear ducts to keep natural tears from draining away. Temporary collagen plugs last 3-6 months. Permanent silicone ones can last years. Studies show they boost tear volume by 40-50%.
Lifestyle Fixes You Can Start Today
Medications aren’t the whole story. Your environment and habits can either make dry eyes worse-or help them heal.
- Use a humidifier-keeping indoor humidity between 40-60% cuts tear evaporation by 25%. This is especially helpful in winter or in air-conditioned spaces.
- Follow the 20-20-20 rule-every 20 minutes, look at something 20 feet away for 20 seconds. For people on antidepressants or antihistamines, this reduces digital eye strain by 35%.
- Block airflow-don’t sit directly in front of fans, car vents, or AC units. Air moving faster than 0.15 m/s over your eyes doubles evaporation. Adjust your seat or redirect the airflow.
- Take omega-3s-1,000 to 2,000 mg of EPA/DHA daily improves tear film stability in 60% of users within 3 months. Look for fish oil or algal oil supplements. This is especially helpful if you’re on diuretics.
- Quit smoking-smoke increases dry eye symptoms by 45% in people on medications. Most notice improvement in 2-4 weeks after quitting.
- Warm compresses-apply a warm, damp cloth to your eyelids for 10-15 minutes twice a day, then gently massage your eyelashes. This melts clogged oil in the meibomian glands. Studies show it helps 65% of people with drug-related gland damage.
When to Talk to Your Doctor
You shouldn’t stop your medication on your own. But you also shouldn’t suffer silently.
Ask your doctor:
- Is there an alternative drug with fewer eye side effects?
- Can the dose be lowered without losing effectiveness?
- Are there preservative-free versions of my eye drops?
For example, switching from a BAK-preserved glaucoma drop to a preservative-free version cuts dry eye complaints from 47% to 16%. And for some people on antidepressants, switching from sertraline to bupropion (Wellbutrin) reduces dry eye risk because it doesn’t have strong anticholinergic effects.
A 2023 study from Richmond Eye Associates found that 55% of patients had symptom relief just from dose adjustments-not even changing the drug. The key? Talking to both your prescribing doctor and your eye specialist together. Coordinated care makes all the difference.
What Doesn’t Work (And Why)
Many people try home remedies that sound good but don’t help-or even hurt.
- Using preserved eye drops too often-more than 4 times a day? You’re adding chemicals that irritate your eyes further.
- Rubbing your eyes-this worsens inflammation and can scratch the cornea.
- Drinking more water alone-while hydration helps, it won’t fix gland damage or nerve-blocking drugs. You need targeted care.
- Waiting for it to get better on its own-dry eye from meds rarely reverses without intervention. The longer you wait, the more damage accumulates.
What’s New in 2026
The field is moving fast. In January 2023, the FDA approved Cequa, a new cyclosporine formula with nanomicellar tech that delivers more medicine to the eye. Clinical trials are now testing lipid-based emulsions specifically for people on isotretinoin-with early results showing 40% improvement in tear stability after just 8 weeks.
Insurance coverage is still a hurdle. Restasis costs around $550/month in the U.S., and many plans don’t cover dry eye treatments. But preservative-free artificial tears are now 35% of the market-up from 15% in 2018-because demand is growing. More doctors are using diagnostic tools like tear osmolarity tests and meibomian gland imaging to personalize treatment.
One thing’s clear: dry eye from medications isn’t just a side effect-it’s a signal. Your body is telling you something’s off. And with the right mix of lubrication, lifestyle tweaks, and medical teamwork, you can protect your vision and your comfort.
Can I stop my medication if it’s causing dry eyes?
No-not without talking to your doctor. Stopping blood pressure meds, antidepressants, or chemotherapy abruptly can be dangerous. Instead, ask if there’s an alternative drug with fewer eye side effects, or if your dose can be lowered. Many patients see improvement with small changes, not full discontinuation.
Are preservative-free eye drops worth the extra cost?
Yes-if you’re using them more than 3-4 times a day. Preservatives like BAK can damage your eye surface over time, making dryness worse. Preservative-free drops are designed for frequent use and don’t carry that risk. While they cost more per bottle, you’ll need fewer bottles overall because they last longer (single-use vials don’t expire after opening).
How long until I feel better after starting treatment?
You may notice less irritation within 1-2 weeks of switching to preservative-free tears and using warm compresses. But treatments like cyclosporine (Restasis) or lifitegrast (Xiidra) take 3-6 months to show full effect. Consistency matters more than speed-stick with the routine even if you don’t feel immediate relief.
Can omega-3 supplements really help with dry eyes from meds?
Yes, especially if your meds cause dehydration or gland damage. Omega-3s (EPA/DHA) improve the quality of your tear’s oil layer, helping it last longer. Studies show 60% of users see better tear stability after 3 months of taking 1,000-2,000 mg daily. Fish oil or algal oil supplements are best.
Why do glaucoma eye drops cause dry eyes?
Most contain benzalkonium chloride (BAK), a preservative that kills bacteria-but also damages the surface cells of your eye. Over time, this leads to inflammation and reduced tear production. Switching to a preservative-free version cuts dry eye complaints by more than half. Ask your eye doctor if your current drops have BAK.
Andy Cortez
February 8, 2026 AT 06:04Jacob den Hollander
February 8, 2026 AT 22:15Camille Hall
February 10, 2026 AT 21:20Monica Warnick
February 11, 2026 AT 06:12Ashlyn Ellison
February 11, 2026 AT 08:27Chelsea Deflyss
February 12, 2026 AT 06:30Tricia O'Sullivan
February 13, 2026 AT 23:21Alex Ogle
February 15, 2026 AT 06:48Tasha Lake
February 16, 2026 AT 18:56Brett Pouser
February 16, 2026 AT 21:40Karianne Jackson
February 17, 2026 AT 09:55glenn mendoza
February 17, 2026 AT 23:33Tori Thenazi
February 18, 2026 AT 11:04Angie Datuin
February 19, 2026 AT 01:39Ritteka Goyal
February 20, 2026 AT 22:52