Eye Swelling and Diabetes: Essential Facts & Prevention Tips
Blood Sugar to Fluid Retention Calculator
High blood sugar can disrupt fluid balance, leading to eye swelling. Estimate how much fluid retention might occur based on your blood sugar level.
How this relates to eye swelling:
When blood sugar levels rise above normal, the kidneys filter more blood, pulling water and electrolytes into urine. This can trigger rebound fluid retention once sugar levels drop, especially in the delicate tissues around the eyes.
Practical Advice
- Prevention Keep blood sugar within target range (A1C < 7%)
- Prevention Reduce salt intake
- Prevention Use cold compresses for mild swelling
- Action Contact your doctor if swelling is sudden or accompanied by vision changes
Eye Swelling is the accumulation of fluid in the tissues around the eye, causing puffiness, redness, and sometimes pain that can be alarming for anyone, but it becomes a bigger red flag when you also have Diabetes is a chronic metabolic condition characterized by high blood glucose levels due to insulin deficiency or resistance. If you’ve been diagnosed with diabetes and notice your eyelids or the skin around your eyes looking puffy, you’re probably wondering whether the two are linked, what the underlying mechanisms are, and how you can keep the swelling under control. Below you’ll find a straight‑forward guide that walks you through the science, the symptoms to watch, and practical steps you can start today.
Key Takeaways
- High blood sugar can disturb fluid balance, leading to periorbital edema.
- Vascular damage and nerve impairment in diabetes make the eye tissues more prone to inflammation.
- Common diabetic eye conditions that cause swelling include blepharitis, allergic conjunctivitis, and diabetic macular edema.
- Controlling glucose, reducing salt, and maintaining good eye hygiene are the most effective preventive measures.
- Seek professional care if swelling is sudden, painful, or accompanied by vision changes.
How Diabetes Triggers Eye Swelling
Diabetes affects almost every part of the body, and the eyes are no exception. Three main pathways explain why fluid starts to pool around the eyes:
- Blood‑sugar spikes and fluid balance: When glucose levels soar, the kidneys filter more blood, pulling extra water and electrolytes into the urine. This diuretic effect can trigger a rebound retention of fluid once the sugar level drops, especially in the delicate tissues around the eyes.
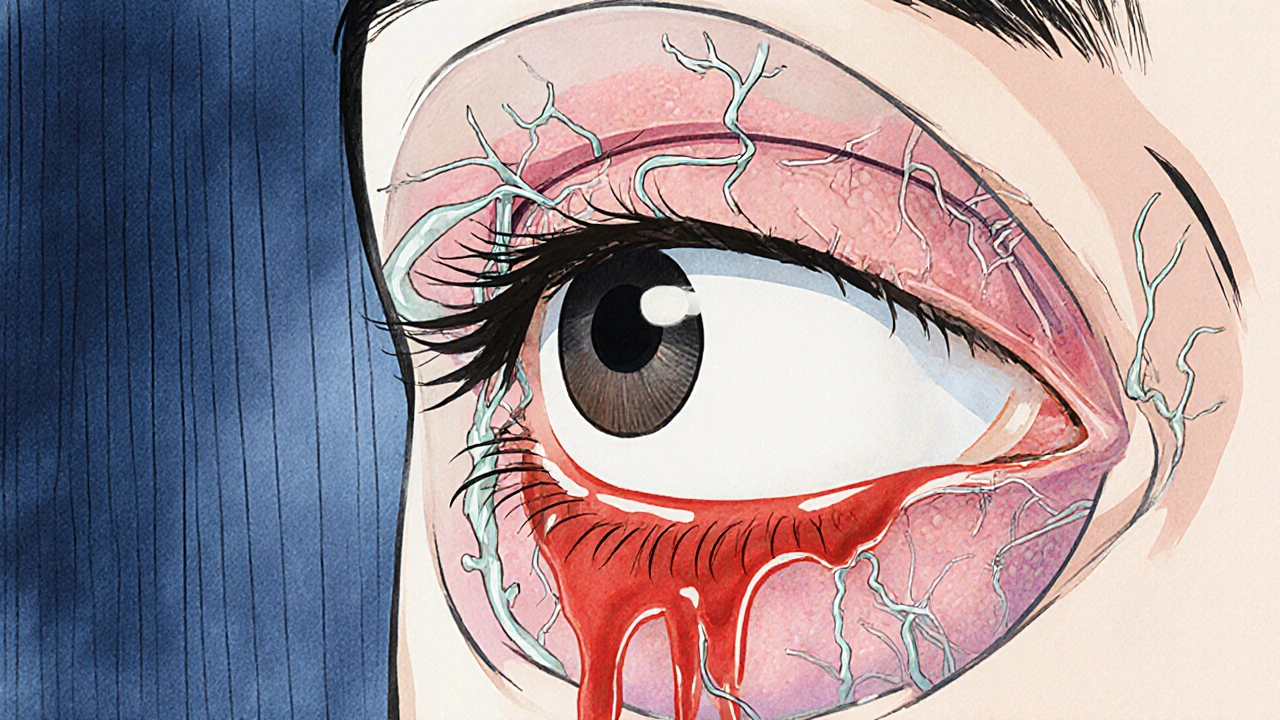
- Vascular changes: Chronic hyperglycemia damages the tiny blood vessels (microangiopathy). Leaky capillaries let plasma seep into surrounding tissue, creating a puffy appearance known as periorbital edema.
- Nerve damage (neuropathy): Diabetic neuropathy reduces the ability of the autonomic nervous system to regulate blood‑vessel tone, further compromising fluid drainage from the eyelids.
These mechanisms don’t work in isolation; they amplify each other, making diabetics more susceptible to swelling even with modest sugar fluctuations.
Common Types of Eye Swelling in Diabetics
Not every puffiness is the same. Understanding the specific condition helps you choose the right treatment.
- Blepharitis: Inflammation of the eyelid margins caused by bacterial overgrowth or oil gland blockage. Diabetics often experience dry eye, which can worsen blepharitis.
- Allergic Conjunctivitis: While allergies affect anyone, high blood‑sugar levels can heighten the immune response, making the eyes more reactive to pollen, dust, or pet dander.
- Diabetic Macular Edema (DME): Fluid builds up in the macula, the central part of the retina. Though DME primarily affects vision, swelling surrounding the eye can sometimes be noticeable.
- Periorbital Edema: Generalized puffiness of the skin around the eye, often a direct result of the vascular leakage described above.
When to Seek Medical Help
If you notice any of the following, schedule an eye‑care appointment promptly:
- Sudden, painful swelling that doesn’t improve with a cold compress.
- Redness spreading beyond the eyelid margins.
- Blurred or double vision, especially if accompanied by swelling.
- Persistent discharge, crusting, or a feeling of a foreign body.
- Swelling that recurs despite good blood‑sugar control.
These symptoms could signal infection, worsening diabetic retinopathy, or an underlying systemic issue such as hypertension.
Managing and Preventing Swelling
Effective management blends medical oversight with everyday habits.
1. Tight Glucose Control
The most powerful tool is keeping your A1C within target range (usually <7%). Consistent monitoring, the right mix of insulin or oral agents, and regular check‑ins with your endocrinologist lower the risk of fluid‑leakage events.
2. Watch Your Salt Intake
Excess sodium forces the body to retain water. Aim for less than 2,300 mg a day, focusing on fresh fruits, vegetables, and low‑sodium versions of processed foods.
3. Stay Hydrated
Paradoxically, drinking enough water helps flush excess sodium and reduces edema. Aim for ~2 L daily, adjusted for activity level and climate.
4. Eye‑Hygiene Routine
- Warm compresses (5 minutes, twice a day) to loosen crusts from blepharitis.
- Gentle lid scrubs using diluted baby shampoo or over‑the‑counter lid cleansers.
- Artificial tears without preservatives if you have dry eye, a common side‑effect of diabetic medication.
5. Medications & Treatments
Only use prescription drops, antihistamines, or steroids under a doctor’s guidance. In cases of DME, anti‑VEGF injections or laser therapy may be recommended.
6. Lifestyle Tweaks
Regular aerobic exercise improves circulation and insulin sensitivity, both of which help keep fluid where it belongs.

Comparison Table: Causes of Eye Swelling - Diabetic vs Non‑diabetic
| Trigger | Diabetic Context | Non‑diabetic Context |
|---|---|---|
| Fluid Retention | Hyperglycemia‑induced vascular leakage | High sodium diet, heart failure |
| Inflammation | Blepharitis linked to dry eye from autonomic neuropathy | Allergic reactions, eczema |
| Infection | \nHigher risk due to impaired immunity | Typical bacterial or viral conjunctivitis |
| Retinal Edema | Diabetic macular edema (fluid in macula) | Age‑related macular degeneration, uveitis |
Quick Checklist for Daily Eye Care
- Check blood‑sugar readings at least twice a day.
- Apply a warm compress to lids each morning.
- Use preservative‑free artificial tears if eyes feel gritty.
- Limit salty snacks and processed foods.
- Stay hydrated - sip water throughout the day.
- Schedule a comprehensive eye exam with an ophthalmologist at least once a year.
Frequently Asked Questions
Can eye swelling be the first sign of diabetes?
Sometimes. Persistent periorbital edema without a clear allergy or infection can prompt a doctor to check blood‑sugar levels, especially if other risk factors exist.
Is it safe to use over‑the‑counter antihistamine drops while I have diabetes?
Generally yes, but you should avoid drops that contain preservatives if you have dry eye, a common diabetic side‑effect. Check with your eye‑care professional before starting any new medication.
How quickly can swelling go down after controlling blood sugar?
Mild edema may improve within a few days of stabilizing glucose, while chronic vascular leakage can take weeks or require topical treatment.
Do I need to see an ophthalmologist for every episode of eye swelling?
If swelling is mild, short‑lived, and you have good glucose control, a primary‑care doctor or optometrist can often manage it. Seek an ophthalmologist if vision changes, persistent pain, or signs of diabetic macular edema appear.
Can lifestyle changes alone eliminate eye swelling?
Lifestyle tweaks-balanced diet, regular exercise, reduced sodium, adequate hydration-significantly lower risk, but they complement, not replace, medical treatment when underlying disease is present.
Understanding the link between eye swelling diabetes empowers you to act before the puffiness becomes a bigger problem. Keep a close eye on your blood‑sugar numbers, protect your lids with simple daily habits, and don’t hesitate to get professional help when needed. Your vision and comfort are worth the effort.
Kelly Brammer
October 22, 2025 AT 12:13It is incumbent upon anyone managing diabetes to recognize that ocular health is not a peripheral concern but a central component of overall wellbeing. Persistent periorbital edema is a tangible signal that systemic glucose regulation is suboptimal, and ignoring it borders on negligence. A disciplined regimen of blood‑sugar monitoring, coupled with a low‑sodium diet, can dramatically reduce fluid accumulation around the eyes. Moreover, regular ophthalmologic examinations should be scheduled at least annually to detect early signs of macular edema or blepharitis. In short, treating eye swelling as merely cosmetic undermines the moral responsibility we all share to protect our bodies.
Gary Marks
November 3, 2025 AT 01:00Honestly, this article reads like a bland pamphlet written by someone who never had to battle the relentless chaos of uncontrolled diabetes. The whole “tight glucose control” mantra is tossed around like a tired cliché, and anyone with a modicum of experience knows that real life is far messier. You scribble “reduce salt” and expect miracles-like salt is the grand puppeteer pulling the strings of periorbital edema, a notion so simplistic it borders on naive propaganda. Your list of “common types of eye swelling” feels like a half‑hearted bullet‑point cheat sheet, a lazy shortcut that pretends to inform while actually pandering. And let’s not forget the relentless push for cold compresses, as if a bag of frozen peas can magically reverse the vascular damage wrought by years of hyperglycemia. The tone is smug, the advice is generic, and the entire piece is drenched in corporate‑friendly optimism that does nothing to empower the struggling reader. You ignore the socioeconomic barriers that prevent many diabetics from affording regular eye exams, the very reality that turns these “preventive tips” into an unattainable luxury. Moreover, the article drifts lazily over the psychological toll of constantly monitoring blood sugar, a factor that can exacerbate stress‑induced inflammation and, by extension, eye swelling. It’s as if you’re content to slap a Band‑Aid on a gaping wound and call it a day. The aggressive marketing of “tight glucose control” as a silver bullet is a disservice, masking the fact that individualized treatment plans are essential. Your mention of “seek professional care” is the only flicker of genuine concern, but it’s buried beneath a mountain of fluff. The reader is left with a false sense of security, thinking that a quick dash to the pharmacy for antihistamine drops will cure the underlying microvascular havoc. In reality, the battle is far more complex, demanding coordinated care among endocrinologists, ophthalmologists, and nutritionists. This article, with its superficial gloss, does a disservice to the very community it claims to help. It’s a lazy, over‑simplified narrative that panders to the lowest common denominator while ignoring the nuance that truly matters. In short, quit sugar‑coating the grim reality and start delivering hard‑won, actionable insight-if you have any ounce of integrity left.
Vandermolen Willis
November 14, 2025 AT 14:46Great rundown! I’ve found that keeping a consistent sleep schedule and staying hydrated really helps my eyes feel less puffy 😊. Adding a gentle eyelid massage before bedtime can boost circulation and ease that annoying swelling. Remember, a little self‑care goes a long way, so don’t skip those regular eye check‑ups! 👀
Mary Keenan
November 26, 2025 AT 04:33Stop ignoring the swelling-it’s a red flag.
Steven Young
December 7, 2025 AT 18:20They want you to believe it’s just sugar spikes but the real agenda is hidden behind the pharma lobby they never mention. Every time you read about “tight glucose control” you’re being fed a narrative that benefits big corporations. Wake up to the fact that the medical establishment is protecting its profits not your eyesight
Ben Collins
December 19, 2025 AT 08:06Oh, absolutely, because we all have the time and resources to schedule annual eye exams while juggling work, kids, and the endless list of diabetes appointments-sarcasm aside, kudos for the reminder. If you’ve ever tried the cold compress hack, you know it’s not a miracle, but it can be a decent stop‑gap while you wait for professional care. Just remember to pair it with proper glucose monitoring and a low‑salt diet, otherwise you’re basically building a house on sand.
Denver Bright
December 30, 2025 AT 21:53i’m not sure if i’m overstepping but i think we should also consider the emotional stress that comes from dealing with chronic illness, it’s an angle that often gets sidelined.
Kelli Benedik
January 11, 2026 AT 11:40OMG, I totally feel you! 😭 The swelling makes me look like I haven’t slept in weeks, and the mirror just screams “help!” 😩 Trust me, the eyelid massage is my secret weapon, and the cold compress is like a magical freeze‑frame of relief. Keep fighting, we’ve got this! ✨
cariletta jones
January 23, 2026 AT 01:26Every small step counts. Stay positive and keep monitoring your eyes. You’ll get through this.
Kevin Hylant
February 3, 2026 AT 15:13It’s clear that hidden motives exist and the system can be biased. We must stay vigilant and demand transparent care. Our eyes deserve honest attention.