Fibromyalgia Pain: How Antidepressants Help Manage Widespread Chronic Pain

Widespread pain that never seems to go away-burning, aching, throbbing-all over your body, day after day. That’s fibromyalgia for millions of people. It’s not arthritis. It’s not a muscle injury. There’s no swelling, no torn ligaments, no visible damage on an X-ray. Yet the pain is real, constant, and often disabling. For many, the answer doesn’t come from surgery or anti-inflammatories. It comes from medications originally designed to treat depression: antidepressants.
What Makes Fibromyalgia Pain Different?
Fibromyalgia pain isn’t localized. It doesn’t stay in one joint or one muscle group. It moves. It spreads. You might wake up with pain in your neck, feel it in your lower back by lunch, and by evening, your knees and shoulders are on fire. The American College of Rheumatology defines it as pain lasting at least three months, present on both sides of the body and above and below the waist. That’s not just bad days-it’s your new normal. The problem isn’t your muscles or joints. It’s your brain and spinal cord. Research shows the central nervous system in people with fibromyalgia amplifies pain signals. It’s like turning up the volume on a radio that’s already too loud. A light touch that shouldn’t hurt feels like a pinch. A minor ache feels like a stab. This is called central sensitization. It’s why ibuprofen often does nothing, but a low-dose antidepressant can make a difference.Why Antidepressants? They’re Not Just for Mood
It’s a common misunderstanding. If you’re not depressed, why are you being prescribed an antidepressant? The answer is simple: these drugs work on pain pathways, not just mood. Serotonin and norepinephrine are brain chemicals that help regulate how your nervous system processes pain. Antidepressants boost these chemicals, effectively quieting the noise in your nervous system. Three types are most commonly used:- Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline-low doses (5-50 mg) at bedtime
- SNRIs like duloxetine (Cymbalta) and milnacipran (Savella)-standard doses for pain, not depression
- SSRIs like fluoxetine-less effective for pain, sometimes used for mood support
How Well Do They Really Work?
Let’s be honest: antidepressants aren’t magic. They don’t make the pain vanish. But they can turn an 8 out of 10 down to a 5. That’s life-changing. Studies show about half of people with fibromyalgia get at least a 30% reduction in pain. Around 10-20% see a 50% drop. That might sound low, but for someone who’s been in constant pain for years, even a 30% improvement means you can finally sleep through the night, take a walk without collapsing, or play with your kids without crying afterward. Amitriptyline stands out for sleep. In one study, 35% of users reported fewer sleep disturbances. SNRIs like duloxetine are better tolerated but less effective at improving sleep. Milnacipran gives more energy, which helps people return to daily tasks. But it often causes headaches. Side effects are real. Dry mouth (68% with amitriptyline), nausea (49% with duloxetine), dizziness, weight gain, fatigue. About 30% of people quit within three months because the side effects feel worse than the pain.It Takes Time-And Patience
You won’t feel better after a week. Or even two. Antidepressants for pain take 4 to 8 weeks to work. Some need up to 12. That’s hard when you’re already exhausted. Many patients give up too soon. Doctors start low and go slow. Amitriptyline? Often begin with 5 mg at night-half a pill. Increase by 5 mg every week. Duloxetine? Start at 30 mg, then bump to 60 mg after two weeks. The goal isn’t to hit the maximum dose fast. It’s to find the lowest dose that helps, without making you feel awful. If you don’t see at least a 20% pain reduction after 6-8 weeks at the target dose, the drug likely won’t help you. That’s when you and your doctor talk about switching.
Who Benefits Most?
Not everyone responds the same. Antidepressants work best if you have:- Significant sleep problems
- Depression or anxiety (which affects 30-50% of fibromyalgia patients)
- Pain that worsens with stress
Real People, Real Experiences
Reddit threads and patient reviews tell the real story:- “Amitriptyline at 10 mg finally let me sleep through the night after 8 years. Dry mouth? Brutal. Worth it.” - u/FibroWarrior87
- “Duloxetine cut my pain from 8/10 to 5/10. But I felt emotionally flat. Like I lost a part of myself.” - u/PainFreeFuture
- “Milnacipran gave me the energy to care for my kids. Headache? Constant. Switched after two months.” - u/FibroMom
Antidepressants Are Just One Piece
No doctor worth their license will tell you to rely only on pills. The CDC, Arthritis Foundation, and European guidelines all agree: exercise is the most effective treatment for fibromyalgia. Walking, swimming, yoga, tai chi-anything that moves you gently but consistently-reduces pain more than any drug. Stress management, good sleep hygiene, and cognitive behavioral therapy (CBT) also help retrain your brain’s response to pain. Antidepressants work best when paired with these. Think of them as a tool, not a cure. They give you enough relief to get moving, to start therapy, to rebuild your life.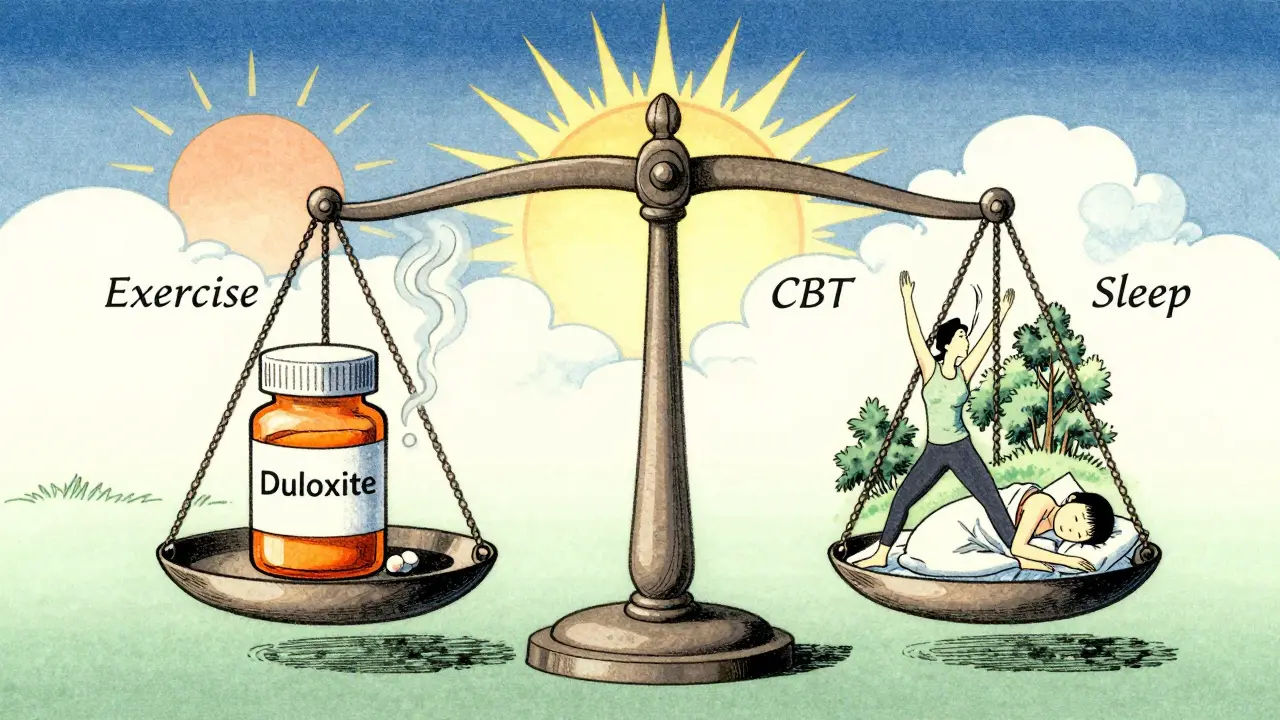
What’s Next?
New drugs are coming, but slowly. One experimental medication, capivasertib, is in late-stage trials. Researchers are also exploring drugs that target NMDA receptors, which play a role in pain amplification. Early results show promise. For now, the focus is on using what we have better. Genetic testing for liver enzymes (CYP450) can now help predict who will tolerate certain antidepressants. Some clinics use the “3-3-3 rule”: start at 3 mg, increase by 3 mg every 3 days. It’s slow, but it cuts side effects. The future isn’t about a miracle pill. It’s about personalized, multimodal care. Antidepressants are part of that. Not the whole story.Key Takeaways
- Fibromyalgia pain is caused by nervous system overactivity, not tissue damage.
- Antidepressants like amitriptyline, duloxetine, and milnacipran reduce pain by modulating brain chemicals.
- They take 4-12 weeks to work-don’t quit too soon.
- Only about half of users get meaningful pain relief; 10-20% get 50% improvement.
- Side effects are common and often lead to discontinuation.
- They work best when combined with exercise, sleep improvement, and stress management.
- Low-dose TCAs are the most cost-effective; SNRIs are better tolerated.
Can antidepressants cure fibromyalgia?
No. Fibromyalgia has no known cure. Antidepressants help manage symptoms-mainly pain, sleep, and mood-but they don’t fix the underlying nervous system dysfunction. Treatment goals are about improving quality of life, not eliminating the condition.
Why use a low dose if it’s an antidepressant?
For pain, you need much lower doses than for depression. Amitriptyline for fibromyalgia is usually 5-50 mg, while depression treatment often starts at 75-100 mg. The pain-relieving effect happens at doses too low to significantly affect mood.
What if I’m not depressed? Do I still need to take an antidepressant?
Yes. These medications work on pain pathways regardless of your mood. Many people without depression benefit from them. The label says “antidepressant,” but the mechanism for pain relief is separate from treating depression.
Are there alternatives to antidepressants for fibromyalgia pain?
Yes. Pregabalin (Lyrica) and gabapentin are FDA-approved for fibromyalgia and work differently-by calming overactive nerves. Non-drug options include aerobic exercise, CBT, acupuncture, and mindfulness. Many people use a mix of these with or without medication.
How do I know if an antidepressant is working for me?
Track your pain on a scale of 1-10 daily for 6-8 weeks. Note sleep quality, energy levels, and mood. If your average pain drops by 20% or more, and you can do more daily activities without exhaustion, it’s likely helping. If not, talk to your doctor about adjusting or switching.
Can I stop taking antidepressants once I feel better?
Don’t stop suddenly. Even if you feel better, taper off slowly under medical supervision. Stopping abruptly can cause withdrawal symptoms like dizziness, nausea, or worsening pain. Many people stay on low doses long-term because fibromyalgia is chronic. Maintenance doses are often lower than initial treatment doses.
What to Do Next
If you’re considering antidepressants for fibromyalgia:- Start with non-drug approaches: walk 20 minutes a day, improve sleep routine, reduce stress.
- Track your pain and symptoms for two weeks. Use a simple journal or app.
- Talk to your doctor about amitriptyline or duloxetine. Ask about starting low and going slow.
- Give it at least 6 weeks before deciding if it works.
- Keep moving. Exercise is the most powerful tool you have.
Paul Ong
January 3, 2026 AT 08:59Been on amitriptyline for 3 years now at 10mg
Woke up without screaming for the first time in a decade
Dry mouth? Yeah but I can actually brush my teeth now
Worth every second
Phoebe McKenzie
January 5, 2026 AT 05:38Of course the medical industry pushes antidepressants for pain-pharma owns everything
They don’t want you cured they want you dependent
Exercise? Sleep? That doesn’t make them billions
It’s all a scam wrapped in a white coat
Stephen Gikuma
January 5, 2026 AT 18:35Antidepressants? That’s what they gave my cousin after 9/11
Now she’s on six meds and can’t remember her own kids
They’re drugging the pain away instead of fixing the system
They don’t care about us, they care about profits
Bobby Collins
January 6, 2026 AT 17:48wait so you're telling me the government is using antidepressants to control chronic pain patients??
like... are they trying to keep us docile??
im not taking anything anymore
LIZETH DE PACHECO
January 7, 2026 AT 07:04Hey I’ve been there-pain so bad you cry just rolling over
Started with 5mg amitriptyline like the post said
Took 6 weeks but now I can hug my niece without wanting to die
It’s not magic but it’s real
Don’t give up before it has a chance
sharad vyas
January 7, 2026 AT 23:11In India we call this mind-body connection
Not medicine, but balance
When mind is loud, body screams
Antidepressants quiet the mind
But yoga and breath quiet the soul
Both help, one just comes faster
Andy Heinlein
January 9, 2026 AT 01:17just started duloxetine last week
still feel like a zombie but my knees stopped screaming at night
gotta give it time
also walking 10 mins a day feels like a win now
small steps right??
Austin Mac-Anabraba
January 9, 2026 AT 15:22The data is statistically insignificant. 30% pain reduction? That’s placebo territory.
Central sensitization is a buzzword, not a mechanism.
You’re replacing one pharmacological illusion with another.
Exercise doesn’t ‘cure’ anything-it just distracts.
And you call this medicine? This is behavioral management disguised as science.
gerard najera
January 10, 2026 AT 22:19It works.
Not perfect.
But better than nothing.
Layla Anna
January 12, 2026 AT 10:39my mom tried amitriptyline and said her sleep improved but she felt like a robot
she cried one night because she couldn't feel joy anymore
we switched to yoga and now she's smiling again
meds help some... but not all
you're not broken, you're just out of balance :)
Heather Josey
January 13, 2026 AT 04:17I appreciate the thorough breakdown of medication efficacy and side effects.
It’s critical to emphasize that antidepressants are adjunctive, not curative.
Combining pharmacological support with CBT and graded exercise yields the most sustainable outcomes.
Thank you for presenting evidence-based, patient-centered information.
Donna Peplinskie
January 14, 2026 AT 07:27Oh my gosh, this is so helpful!!
I’ve been struggling for years and no one ever explained why antidepressants were even an option...
Now I get it-it’s not about being sad, it’s about the noise in your brain being too loud!
And the part about starting low?? That’s the key I was missing!!
Thank you for writing this so clearly-I’m going to share it with my whole family!!
jaspreet sandhu
January 15, 2026 AT 19:47Why do you think only Americans rely on pills for everything
In my village in Punjab we use turmeric and massage and prayer
Why do you need a pill to fix what your body can heal itself
You have too many doctors and too little faith
Antidepressants are a crutch for people who don’t want to sit with their pain
It’s easier to swallow a pill than to change your life
Alex Warden
January 16, 2026 AT 08:13They’re drugging the working class to keep them quiet
While CEOs get rich off the pain industry
Why don’t they fix the jobs that break people
Why don’t they fix the stress
Why do we need a pill just to get through the day
This ain’t healthcare, this is control