First-Generation Antihistamines: Why Severe Drowsiness and Anticholinergic Effects Matter

Drowsiness Duration Calculator
Estimate how long drowsiness may last after taking first-generation antihistamines like Benadryl. Based on data from clinical studies showing effects up to 18 hours.
Enter your information to calculate drowsiness duration.
Many people reach for diphenhydramine (Benadryl) or chlorpheniramine (Chlor-Trimeton) when they have allergies, a cold, or trouble sleeping. It’s cheap, easy to find, and works fast. But what they don’t realize is that these first-generation antihistamines aren’t just blocking histamine-they’re also flooding the brain with side effects that can last all day, even after the allergy symptoms fade.
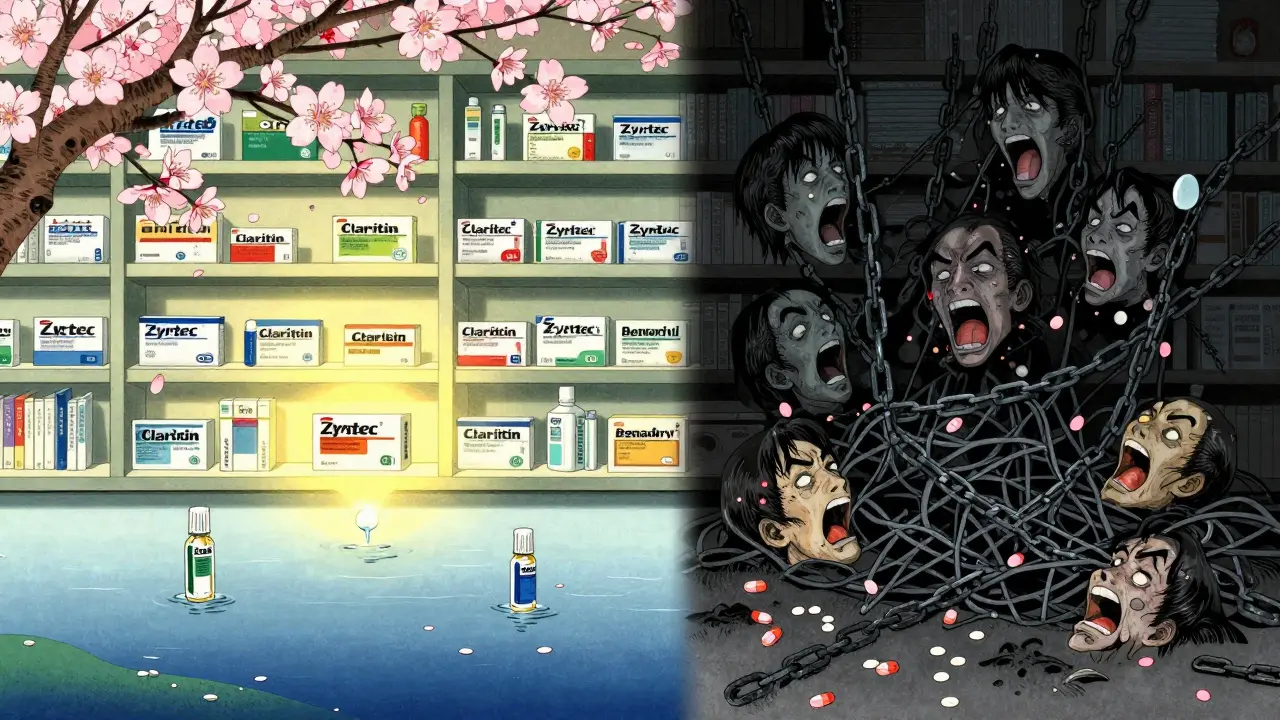
Why You Feel Like a Zombie After Taking Benadryl
First-generation antihistamines like diphenhydramine, promethazine, and hydroxyzine are designed to block histamine receptors, but they don’t stop there. Their chemical structure is small and oily, which lets them slip easily through the blood-brain barrier. Once inside the brain, they bind to H1 receptors in areas that control wakefulness, attention, and memory. The result? Severe drowsiness. Not just a little sleepy-full-on brain fog.
Studies show that within 1 to 2 hours of taking a standard 25 mg dose of diphenhydramine, brain concentrations hit 15-25 ng/mL. That’s enough to impair reaction time as much as having a blood alcohol level of 0.05%. Driving simulators show performance drops by 70-90% compared to placebo. And it’s not just temporary. In one study, cognitive impairment lasted up to 18 hours after a single dose. That means if you take it at 8 p.m. to help you sleep, you might still feel sluggish at noon the next day.
The Hidden Anticholinergic Toll
What makes these drugs even more dangerous is their side effect profile beyond sleepiness. They don’t just block histamine-they also bind tightly to muscarinic receptors, which are part of the parasympathetic nervous system. This is called anticholinergic activity. It’s why you get dry mouth, blurred vision, constipation, urinary retention, and confusion.
These aren’t minor annoyances. Dry mouth can lead to dental decay. Blurred vision increases fall risk, especially in older adults. Urinary retention can require emergency catheterization. And cognitive impairment? It’s not just feeling slow-it’s measurable memory loss. Long-term use of first-generation antihistamines is linked to a 54% higher risk of dementia in people over 65, according to the American Geriatrics Society’s Beers Criteria. That’s why they’re listed as potentially inappropriate medications for seniors.
Who’s Still Using Them-and Why
Despite the risks, millions of Americans still use these drugs. Why? Cost. A bottle of 24 diphenhydramine tablets costs around $5. The same number of cetirizine (Zyrtec) tablets runs $15. For people without insurance, the price difference is hard to ignore.
They’re also used for non-allergy reasons. Many take them as a sleep aid because they knock you out fast. Clinical trials show they reduce sleep onset latency by 30-40 minutes. But here’s the catch: they don’t improve sleep quality. They suppress REM sleep, leading to unrefreshing rest. People wake up groggy, with what they call a ‘hangover effect.’ One Reddit user wrote: ‘Took Benadryl at 8 PM for hives and woke up at 2 PM the next day feeling like I’d been hit by a truck.’
They’re also used for motion sickness and nausea. Promethazine is still prescribed for this because it’s one of the few drugs that works reliably for vertigo and vomiting. But again, the trade-off is severe sedation. If you’re on a cruise and take it before boarding, you’ll likely spend the whole trip lying down.

The Data Doesn’t Lie: Real People, Real Side Effects
Look at the reviews. On Drugs.com, diphenhydramine has a 5.2 out of 10 rating from over 3,700 users. Nearly 40% say they experienced ‘extreme sleepiness.’ Over 20% report trouble concentrating. On WebMD forums, 28% of long-term users mention urinary problems-classic anticholinergic effects.
Emergency room data is even more alarming. In 2021, 35% of drowsy driving incidents involving medication were tied to first-generation antihistamines. Kids are getting into trouble too. Between 2018 and 2022, pediatric ER visits for diphenhydramine misuse rose 27%. In the UK, promethazine was banned for sale to minors in 2022. The FDA is now considering similar restrictions.
Who Should Avoid Them-and Who Might Still Use Them
If you’re over 65, pregnant, have glaucoma, an enlarged prostate, or a history of dementia, you should avoid these drugs entirely. Even if you’re young and healthy, think twice before using them daily.
There are only a few situations where first-generation antihistamines still make sense:
- Short-term use for motion sickness (70-80% effective)
- Occasional insomnia when other options fail
- Acute allergic reactions where fast action is critical
Even then, use the lowest effective dose-12.5 mg of diphenhydramine instead of 25 mg-and take it at night. Never combine with alcohol, opioids, or benzodiazepines. That combo can suppress breathing.
The Future: Better Options Are Here
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) don’t cross the blood-brain barrier. Their brain concentrations stay below 1 ng/mL. That means they relieve allergies without making you drowsy. Driving studies show they cause almost no impairment.
And they’re getting cheaper. Generic versions of Zyrtec and Claritin now cost under $10 for a month’s supply. Many pharmacies offer them for $4 at Walmart or CVS. The price gap is closing fast.
Even better, new ‘third-generation’ antihistamines are in development. Two candidates, EB-029 and DP-118, are in Phase II trials. They’re designed to block histamine in the body while staying out of the brain entirely. Early results show 80% less CNS penetration-without losing effectiveness.
What to Do Instead
If you’re using diphenhydramine for allergies, switch to a second-generation option. Try cetirizine 10 mg once daily. It works just as well and doesn’t fog your brain.
If you’re using it for sleep, try melatonin (3 mg) or a non-habit-forming sleep aid like doxylamine succinate (Unisom SleepGels)-but only for short-term use. Better yet, fix your sleep hygiene: no screens after 9 p.m., keep your room cool, and get sunlight in the morning.
If you’re using it for nausea or motion sickness, consider ginger supplements or acupressure wristbands. They’re not as fast, but they’re safer for long-term use.
The bottom line? First-generation antihistamines aren’t harmless. They’re powerful drugs with real risks. Just because they’re sold over the counter doesn’t mean they’re safe for everyday use. Treat them like prescription meds-use them wisely, sparingly, and only when the benefits clearly outweigh the cost to your brain.
Are first-generation antihistamines safe for seniors?
No. The American Geriatrics Society strongly advises against using first-generation antihistamines like diphenhydramine in adults over 65. These drugs have strong anticholinergic effects that increase the risk of confusion, falls, urinary retention, and dementia. Chronic use is linked to a 54% higher risk of cognitive decline. Safer alternatives like loratadine or cetirizine are available and should be used instead.
How long does drowsiness last after taking Benadryl?
Drowsiness from diphenhydramine typically starts within 30 minutes and peaks at 1-2 hours. But the effects can last up to 18 hours, especially in older adults or those with slower metabolism. Driving and cognitive tests show impairment lasting well into the next day, even after you feel ‘awake.’ Never assume you’re safe to drive just because you’re no longer sleepy.
Can I take first-generation antihistamines with alcohol?
Never. Alcohol increases the sedative effects of these drugs by 40-60% and raises the risk of respiratory depression, extreme dizziness, and loss of consciousness. Combining them can be deadly, especially in older adults or those taking other CNS depressants like opioids or sleep meds.
Why do first-generation antihistamines cause dry mouth?
They block muscarinic receptors in the salivary glands, which are responsible for producing saliva. This is part of their anticholinergic effect. Dry mouth isn’t just uncomfortable-it increases the risk of tooth decay, gum disease, and oral infections. Drinking water helps, but it doesn’t fix the root cause. Switching to a second-generation antihistamine is the best solution.
Are there any benefits to using first-generation antihistamines over second-generation ones?
Yes-but only in specific cases. First-generation antihistamines are more effective for motion sickness and nausea, with success rates of 70-80% compared to 40-50% for second-generation drugs. They also work faster for acute allergic reactions and can be useful for short-term insomnia. But for daily allergy relief, daytime use, or long-term treatment, second-generation options are far safer and just as effective.
Tom Swinton
January 4, 2026 AT 13:21Look, I get it-Benadryl’s cheap, it works, and yeah, I’ve used it to knock myself out after a rough week. But after reading this, I realized I’ve been treating it like a bedtime tea, not a chemical hammer to the brain. I took it for three nights straight last winter for allergies, and the next day? I forgot where I put my keys. Twice. Then I misread my boss’s email and showed up to a meeting in pajamas. No joke. I thought I was just tired. Turns out, I was half-dead from anticholinergic fog. I switched to Zyrtec last month. No more brain fog. No more dry mouth that feels like chewing sandpaper. I’m not saying it’s magic, but it’s not poisoning me either. Worth the extra $10.
Rachel Wermager
January 5, 2026 AT 04:20Let’s be precise: first-gen antihistamines are non-selective H1 antagonists with high lipophilicity, permitting unrestricted CNS penetration. Their anticholinergic burden is quantifiable via the Anticholinergic Cognitive Burden (ACB) scale-diphenhydramine scores a 3, the highest risk tier. Chronic exposure induces downregulation of muscarinic M1 receptors in the hippocampus, directly correlating with reduced synaptic plasticity and accelerated neurodegeneration. The 54% dementia risk increase isn’t correlation-it’s dose-dependent neurotoxicity. And don’t get me started on the pharmacokinetic variability in elderly patients with reduced CYP2D6 activity. This isn’t ‘just drowsiness.’ It’s iatrogenic cognitive erosion disguised as OTC relief.
Leonard Shit
January 5, 2026 AT 08:14lol i just took benadryl last night for my sneezes... woke up at 4pm feeling like i got run over by a bus made of regret. also my mouth felt like the inside of a desert. i thought it was just bad sleep. turns out i was just slowly dying in slow motion. thanks for the wake up call. also i just googled ‘what is anticholinergic’ and now i’m scared. but also smarter. maybe i’ll try that zyrtec thing. if it doesn’t cost $200.
Wesley Pereira
January 5, 2026 AT 13:03So you’re telling me the thing I’ve been using to ‘sleep’ for 12 years is basically a cognitive tax collector? And I thought my brain was just aging. Nope. It’s been hijacked by a $5 pill that’s basically the pharmaceutical equivalent of a 1998 Nokia battery. I’m switching to cetirizine tomorrow. Also, I’m telling my mom to stop giving her grandkids diphenhydramine ‘for the cough.’ She thinks it’s ‘natural’ because it’s in ‘herbal’ sleep gummies. It’s not natural. It’s a neurotoxin with a marketing team.
Tiffany Adjei - Opong
January 6, 2026 AT 15:47Okay but what if you’re poor? You think I’m gonna pay $15 for Zyrtec when I’m choosing between medicine and groceries? This post reads like a rich person’s guilt trip. I’ve been using Benadryl for 20 years. I’ve never had dementia. My dad took it for 30 years and lived to 89. You’re scaring people with stats while ignoring the real problem-healthcare inequality. Stop blaming the medicine and fix the system. Also, I’m not giving up my $5 sleep aid just because some PhD thinks my brain is melting.
Kiran Plaha
January 7, 2026 AT 19:42in india we use promethazine for motion sickness. my uncle takes it before bus trips. he sleeps the whole ride. no one says anything. but now i wonder-is he okay? i never thought about dry mouth or memory. i thought it was just how it works. maybe i should tell him about zyrtec. but he says ‘if it ain’t broke, don’t fix it.’ i don’t know what to do.
Melanie Clark
January 7, 2026 AT 23:59They don’t want you to know this but the pharmaceutical companies made first-gen antihistamines cheap on purpose so you’d keep using them. Why? Because they make billions off the second-gen drugs. They knew the side effects for decades. They buried the studies. The FDA? Bought and paid for. The dementia link? Not a coincidence. It’s a slow genocide of the elderly so they can sell you memory pills later. Wake up. This isn’t medicine-it’s a profit scheme disguised as healthcare. And your ‘cheap’ Benadryl? It’s a Trojan horse. 🕵️♀️💊
Isaac Jules
January 8, 2026 AT 14:37Wow. So I’ve been poisoning myself for 15 years and now I’m supposed to feel guilty? I’m 28. I take one Benadryl when I’m overwhelmed. I’m not old. I’m not diabetic. I’m not dumb. My brain’s fine. You people act like one pill is going to turn me into a vegetable. I’ve had worse brain fog from binge-watching Netflix. Chill. Also, I’m not paying $15 for something that works for $5. You’re not my mom. Stop scolding me.
Amy Le
January 10, 2026 AT 03:55First-gen antihistamines are the last bastion of American self-reliance. You want to live in a world where every pill is regulated by a panel of elitist doctors? Fine. But I’ll take my $5 sleep aid over your $15 ‘brain-safe’ corporate product any day. This post reads like a corporate ad disguised as public health. Also, I’ve used Benadryl for 20 years and I’ve never missed a day of work. You think I’m stupid? I’m not the one who needs a lecture. I’m the one who gets things done. 🇺🇸
Saylor Frye
January 10, 2026 AT 07:48Oh wow. A 10-page essay on antihistamines. How… academic. I thought this was Reddit. I came here for memes, not a pharmacology lecture. I take Benadryl because it works. I don’t care if it’s ‘neurotoxic’ or ‘anticholinergic’ or whatever. I just want to sleep. Also, I’ve never heard of ‘third-gen’ antihistamines. Are they like, a new iPhone? Are they $500? If so, I’ll stick with my $5 pill. Also, I’m not going to Google ‘muscarinic receptors’ because I have a life.
Katelyn Slack
January 10, 2026 AT 23:01i just wanted to say thank you for writing this. i’m 72 and i’ve been on diphenhydramine for years because my doctor said it was fine. i started forgetting names, having trouble walking, and i thought it was just getting old. i didn’t know it was the medicine. i switched to loratadine last week. my memory’s better. my mouth isn’t dry anymore. i feel like i got my brain back. i wish i’d known sooner.
Stuart Shield
January 12, 2026 AT 10:08Christ, I remember when my grandad used to take that stuff for his hayfever. Said it made him feel ‘like a sleepy sheep.’ We all laughed. Now I know he wasn’t just being poetic-he was describing a slow neurological shutdown. I’ve switched to fexofenadine now. No more ‘sheep mode.’ Just clean, quiet relief. And yeah, it’s a bit pricier. But I’d rather pay for my brain than lose it to a $5 bottle of lies.
Tom Swinton
January 14, 2026 AT 00:00Just read Katelyn’s comment. That hit hard. I’m 31. I’ve been using Benadryl since college. I thought I was fine. But if someone my age can have a wake-up call at 72… what’s my timeline? I’m going to talk to my doctor tomorrow. Not because I’m scared. But because I want to be here-fully awake-for my kid’s first steps. And I don’t want to miss them because I was too lazy to spend $10 on a better pill.