How Humidity and Heat Speed Up Medication Expiration
Most people assume their medications will work exactly as promised-until they don’t. You take a pill past its expiration date, and nothing happens. Or worse, you feel worse. The problem isn’t always that the drug is old. It’s often that it was stored in the wrong place. Heat and humidity are silent killers of medicine potency, and they’re more common in homes than you think.
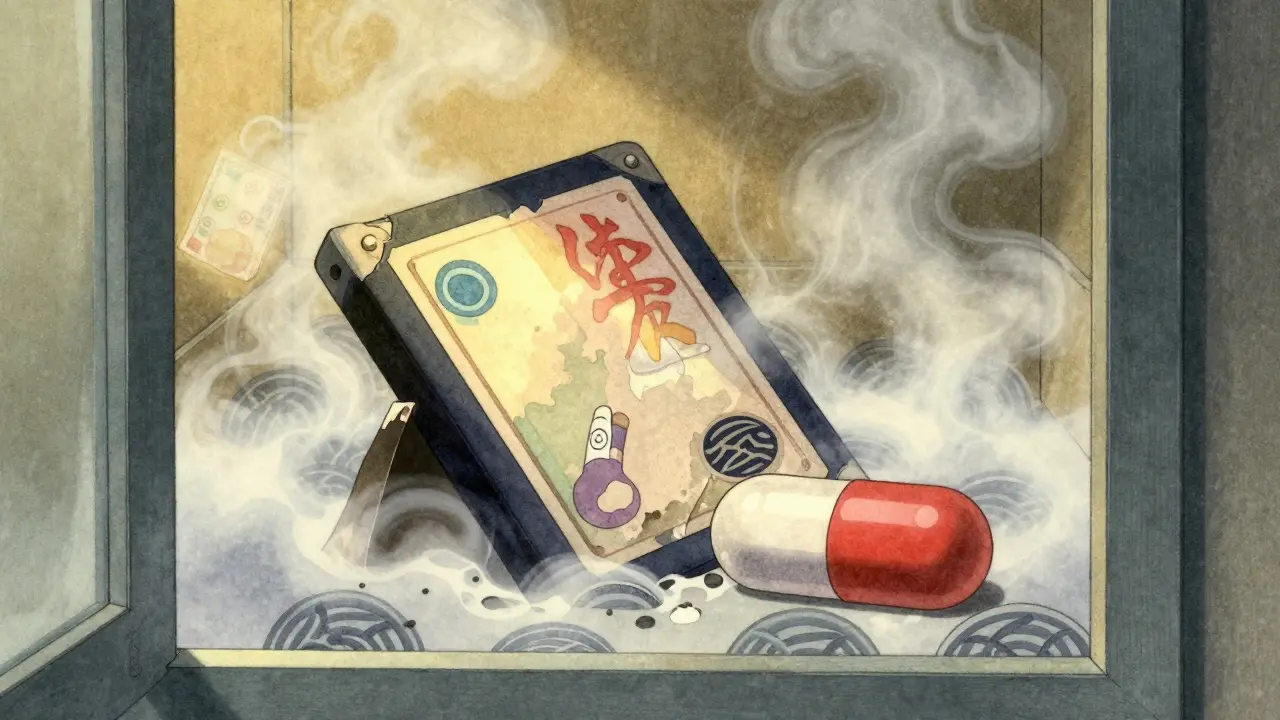
Why Your Medicine Loses Power Before the Date
Expiration dates aren’t arbitrary. They’re the last day a drug is guaranteed to be safe and effective-if stored properly. The pharmaceutical industry tests medications under strict conditions: 20-25°C (68-77°F) and 35-65% humidity. That’s not your bathroom. That’s not your kitchen counter. That’s not your car on a summer day. When heat and moisture sneak in, chemical reactions begin. Tablets can absorb water and swell. Capsules soften and stick together. Liquid medications break down. Insulin molecules unfold. Nitroglycerin turns into useless compounds. These changes don’t always look obvious. You won’t always see a color shift or smell something odd. But the active ingredient? It’s already fading.Which Medications Are Most at Risk?
Not all drugs are created equal when it comes to heat and humidity. Some are tough. Others are fragile. High-risk medications:- Insulin: Loses up to 20% of potency in just 24 hours at 37°C (98.6°F). For diabetics, that means dangerous blood sugar spikes.
- Nitroglycerin: Used for heart attacks. Degrades rapidly above 25°C. A degraded tablet won’t stop chest pain when you need it most.
- Thyroid meds (like levothyroxine): Must stay below 27°C (80.6°F). Even slight heat can throw off your hormone balance.
- Antibiotic suspensions (like amoxicillin): Lose 30-40% potency within 72 hours at room temperature. That’s not just ineffective-it can breed resistant bacteria.
- Biologics (monoclonal antibodies): Protein-based drugs. Once they’re exposed to temperatures above 8°C, their structure collapses. No recovery. No second chances.
- EpiPens: The spring mechanism can fail at 30°C+. You might press it and get nothing. No adrenaline. No rescue.
- Inhalers: Pressurized cans can explode if left in a hot car above 49°C (120°F).
- Acetaminophen tablets
- Ibuprofen pills
- Most statins (like atorvastatin)
- Many antidepressants and blood pressure pills in solid form
Where You’re Actually Storing Your Medicine (And Why It’s Wrong)
The bathroom medicine cabinet is the #1 mistake. It’s humid. It’s warm. After a hot shower, humidity spikes to 70-90%. That’s worse than a rainforest for pills. Moisture gets into bottles. Capsules swell. Tablets crack. Aspirin turns into vinegar and salicylic acid-more irritating to your stomach. The kitchen is almost as bad. Near the sink? Humidity. Near the stove or oven? Temperatures can hit 32°C (90°F) or higher. Even a windowsill above the sink is a chemical reactor. And don’t forget the car. On a sunny day in July, the inside of a parked car can hit 60°C (140°F). That’s hotter than an oven. Medications left there for even an hour can be ruined.
What Heat and Humidity Do to Your Pills (And Why You Can’t Tell)
You might think you can spot bad medicine. You can’t always. Look for these signs:- Tablets that are harder, softer, or crumbly
- Capsules that are stuck together or leaking
- Color changes-yellowing, dark spots
- Unusual smells (like vinegar from aspirin)
- Liquids that look cloudy or have particles
How to Store Medicine Correctly
Follow these rules to keep your meds working:- Keep it cool: 15-25°C (59-77°F) is ideal. A bedroom drawer, a closet shelf, or a dedicated cabinet away from windows works.
- Keep it dry: Never store in bathrooms or kitchens. Use airtight containers if humidity is high.
- Keep it dark: Sunlight breaks down chemicals. Use original opaque bottles. Don’t transfer to clear pill organizers unless you’re using them immediately.
- Keep it sealed: Tight caps prevent moisture from creeping in. Don’t leave bottles open.
- Keep it separate: Don’t mix medications with supplements or vitamins unless you know they’re compatible. Some can react.
- Take only what you need for the trip.
- Use insulated bags with cool packs for insulin, biologics, or nitroglycerin.
- Never leave meds in a car-even if you’re just running in for five minutes.

The Real Danger: What Happens When It Fails
Taking a weakened antibiotic might not kill you-but it could make you sicker. Sub-potent antibiotics don’t kill all the bacteria. The survivors become resistant. That’s how superbugs grow. Insulin that’s lost potency? Your blood sugar goes wild. You could end up in the hospital with ketoacidosis. A failed EpiPen during anaphylaxis? That’s not a medical emergency. That’s a death sentence. Nitroglycerin that doesn’t work during a heart attack? You lose minutes-minutes you won’t get back. The FDA says it plainly: “Using expired medicines is risky and possibly harmful to your health.” It’s not just about potency. It’s about safety.What’s Changing in the Industry
Pharmaceutical companies are starting to respond. New packaging includes desiccants (tiny moisture-absorbing packets), opaque bottles, and temperature-sensitive labels that change color if exposed to heat. Some smart packaging prototypes now have tiny sensors that connect to your phone. If your insulin was stored at 35°C for 3 hours, your app warns you. It’s not mainstream yet-but it’s coming. Meanwhile, climate change is making this worse. Heat waves are longer, hotter, and more frequent. In places like Victoria, Canada, summer temperatures are creeping up. What used to be a rare 30°C day is now common. The World Health Organization calls medication stability in extreme heat a growing public health issue.What You Should Do Right Now
Check your medicine cabinet. Not the one in the bathroom. The one you actually use. Ask yourself:- Is it near a window?
- Is it above the sink or stove?
- Do I leave pills in my purse or car?
- Do I have insulin, nitroglycerin, or EpiPens?
Can I still use medicine after its expiration date if it looks fine?
It’s not safe to assume expired medicine is still good-even if it looks unchanged. Expiration dates are based on stability testing under ideal storage conditions. If your meds were exposed to heat or humidity, they may have lost potency long before the date. Some, like insulin or EpiPens, can become dangerous. When in doubt, throw it out and get a new one.
Is it safe to store pills in a pill organizer for weeks?
Only if you’re using them within a few days. Most pill organizers are clear and open, exposing pills to light, air, and moisture. This can degrade medications faster, especially in humid climates. For daily use, keep your original bottles and use organizers only for short-term travel or daily doses.
Do refrigerated medications need to be kept cold all the time?
It depends. Some, like insulin, can be kept at room temperature (below 25°C) for a limited time after opening-usually 28-30 days. But they must be refrigerated before first use. Biologics and some antibiotics must stay cold at all times. Always check the label or ask your pharmacist. If you’re unsure, keep it cold.
Can heat make medicine toxic?
Yes, in rare cases. Aspirin breaks down into salicylic acid and acetic acid (vinegar), which can irritate the stomach lining. Some antibiotics can form toxic byproducts when degraded. While most expired drugs just lose strength, certain chemicals can become harmful. It’s not common, but the risk exists-especially with older or improperly stored meds.
How do I dispose of expired or damaged medication?
Don’t flush pills or throw them in the trash. Many pharmacies offer take-back programs. In Canada, you can drop off expired or unwanted meds at any pharmacy for safe disposal. Some communities also have drug disposal events. If none are available, mix pills with coffee grounds or cat litter in a sealed bag before tossing-this prevents accidental ingestion and reduces environmental harm.
Jarrod Flesch
January 22, 2026 AT 03:13Just moved all my meds from the bathroom cabinet last month after reading this. Holy crap, I had my insulin sitting right above the shower. 😅 Now it’s in a drawer next to my bed-cool, dry, and out of sight. Feels way less like playing Russian roulette with my blood sugar.
Kelly McRainey Moore
January 22, 2026 AT 13:03I used to keep my EpiPen in my purse-until I left it in my car during a 95°F day. Thank god I didn’t need it then. Now it’s in a small insulated pouch with a cold pack in my fridge. Weird, but I’d rather be safe than sorry. 🤞
Rod Wheatley
January 23, 2026 AT 19:01This is such an important post-seriously, why isn’t this taught in high school? We learn about vitamins and calories, but no one tells you your blood pressure med might turn into paperweight if you leave it on the windowsill. Please share this with your family. Someone’s life could depend on it.
Glenda Marínez Granados
January 25, 2026 AT 15:35So let me get this straight-we’re supposed to treat our medicine like it’s a fine wine… and our bathrooms are the wine cellar from hell? 😏 I’m just glad I never trusted my mom’s ‘medicine cabinet’-she kept Xanax next to the hair dryer. Classic.
michelle Brownsea
January 26, 2026 AT 03:08It’s not just storage-it’s societal negligence. The pharmaceutical industry profits from replacement cycles, and they’ve spent decades normalizing improper storage. The FDA’s warnings are too vague. We need mandatory labeling: ‘DO NOT STORE ABOVE 25°C’ in bold, red, and with a thermometer icon. And yes-I’m serious.
lokesh prasanth
January 27, 2026 AT 08:25heat bad. pills bad. bathroom worst. just keep in drawer. done.
Barbara Mahone
January 28, 2026 AT 22:47I’ve been storing my levothyroxine in a sealed glass jar inside my nightstand since moving to Florida. The humidity here is brutal, and I refuse to risk my TSH levels. It’s not paranoia-it’s precision. And yes, I label the jar with the date I opened it. Because details matter.
Andrew Rinaldi
January 29, 2026 AT 06:51I appreciate how this post doesn’t just scare people-it gives actionable steps. I used to think ‘expiration date’ meant ‘use by’ regardless of environment. Learning that insulin degrades in 24 hours at body temperature… that changed everything. Thanks for the clarity.
Gerard Jordan
January 30, 2026 AT 09:56Just got my first smart pill bottle prototype from my pharmacy. It glows red if it’s been too hot. 🤖💡 I thought it was overkill… until I realized my nephew left his asthma inhaler in the glovebox for three days. Now I’m obsessed. Tech can save lives. 🙌
Samuel Mendoza
January 30, 2026 AT 19:22Most people don’t even know what ‘humidity’ means. They think ‘cool’ means ‘not hot.’ That’s why we have a healthcare crisis.
MAHENDRA MEGHWAL
February 1, 2026 AT 16:26Respected sir, I have observed that in tropical climates, such as in India, the issue of medication degradation is not merely a matter of personal responsibility but a systemic public health concern. Many households lack climate-controlled storage. Government intervention and subsidized desiccant packaging are urgently required.
Coral Bosley
February 2, 2026 AT 16:08I kept my nitro in my purse for two years because I ‘didn’t want to forget it.’ Then one day I realized the bottle felt sticky. I didn’t throw it out-I cried. Then I threw it out. And I bought three new ones. And I’m never doing that again. Ever. Not even if the world ends. 💔