How to Use Label Information to Set Accurate Medication Reminders

Getting your medication schedule right isn’t just about setting an alarm. It’s about understanding what’s written on the label - and using that information to build reminders that actually keep you safe. Too many people set generic alarms for "take pill at 8 AM" and miss the finer details: take with food, wait 2 hours before your other pill, or do not take more than once every 6 hours. When these details are ignored, the risk of side effects, missed doses, or even overdose goes up dramatically. The good news? You don’t need to memorize your label. You just need to know how to read it - and turn it into a smart reminder system.
What’s Really on Your Medication Label?
Your prescription label isn’t just a receipt. It’s a clinical instruction sheet, written under strict FDA guidelines. Every word matters. Here’s what you need to look for:- Dosage form: Is it a tablet, capsule, liquid, or patch? This affects how you take it and how the reminder system should track it.
- Active ingredient and strength: "Lisinopril 10 mg" isn’t the same as "Lisinopril 20 mg." Mixing them up can be dangerous.
- Frequency: "Take one tablet every 8 hours" means three times a day - not just at breakfast, lunch, and dinner. That’s a 24-hour cycle, not a 12-hour one.
- Food instructions: "Take on an empty stomach" means no food for 1 hour before and after. "Take with food" means eat something first - otherwise, the drug might irritate your stomach or not absorb properly.
- Minimum interval: "Do not take more than one dose every 6 hours" is a hard limit. Skipping this rule is how accidental overdoses happen.
- Drug interactions: "Avoid antacids within 2 hours" or "Do not take with grapefruit juice" - these aren’t suggestions. They’re safety rules.
According to a 2023 NIH analysis, 78.3% of timing-related medication errors happen because people ignore or misread these instructions. A reminder that just says "Take pill at 8 AM" doesn’t help if you’re supposed to wait 2 hours after your blood pressure med before taking your cholesterol pill. That’s where smart systems come in.
Why Generic Alarm Apps Fail
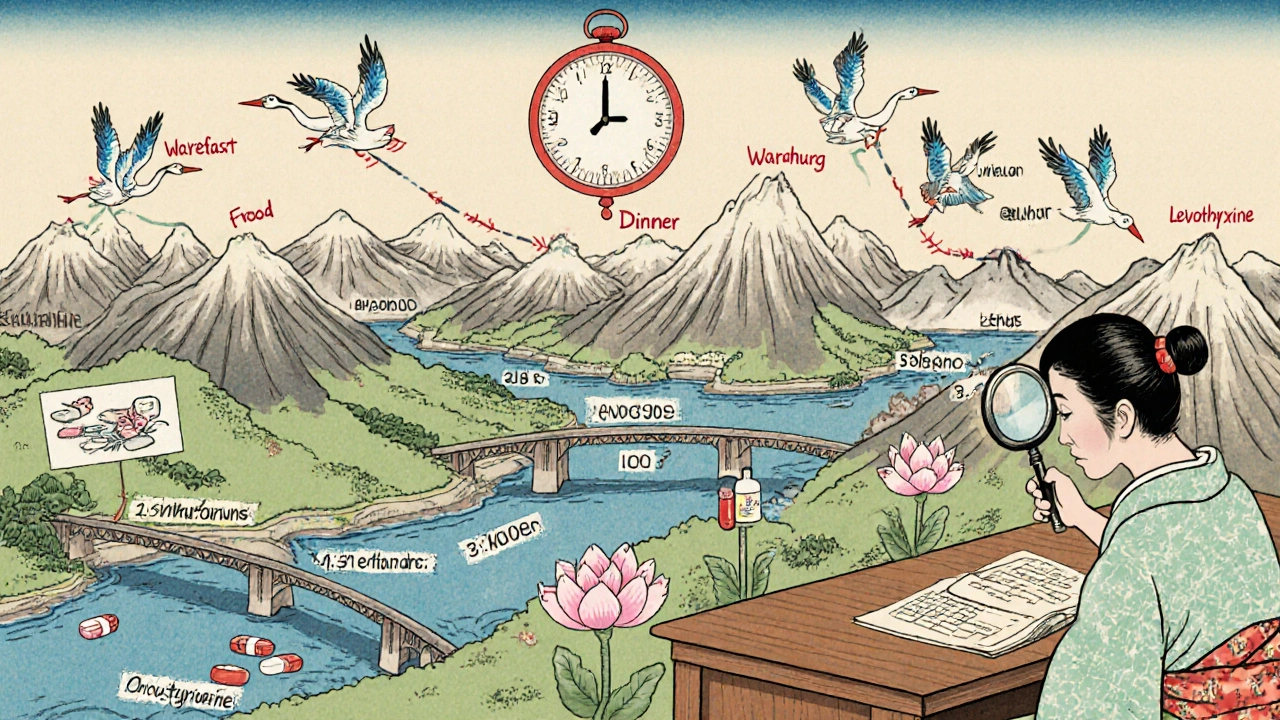
Most phone alarms, simple reminder apps like Alarmy, or even basic pill organizers don’t understand labels. They treat all medications the same: set a time, get a beep. But real medication schedules are layered, overlapping, and conditional.Take a patient on five medications:
- Metformin - take with breakfast
- Atorvastatin - take at bedtime
- Warfarin - take at 6 PM, avoid leafy greens
- Levothyroxine - take on empty stomach, wait 30 minutes before food
- Amoxicillin - take every 8 hours, but not at 2 AM
A basic app might remind you to take all five at 8 AM. That’s wrong. Levothyroxine needs to be taken alone. Warfarin has dietary restrictions. Amoxicillin can’t be taken in the middle of the night. Only a system that reads the label and understands these rules can avoid these mistakes.
A 2024 study in the Journal of Medical Systems compared 12 apps and found that those using label data reduced timing errors by 63.2% compared to generic alarms. Systems like Medisafe and MyTherapy don’t just remind you - they map your entire schedule based on what’s printed on the bottle.
How Smart Systems Turn Labels Into Schedules
Modern medication apps don’t just ask you to type in your meds. They use your label as input. Here’s how it works:- Scan or enter the label: Use your phone’s camera to snap a picture of the label. AI-powered optical character recognition (OCR) reads the text with 98.7% accuracy, according to a 2024 study in npj Digital Medicine.
- Translate instructions: The app converts "take one tablet every 8 hours" into three reminders spaced evenly across 24 hours. "Take with food" becomes a reminder that says "Take with your next meal," not just "8 AM."
- Check for conflicts: The system pulls from a database of over 150,000 drugs and 500,000 interactions. If you’re taking warfarin and amoxicillin, it checks if they interact. If you’re taking levothyroxine and calcium, it warns you to space them by 4 hours.
- Build a visual timeline: Instead of just alarms, you get a daily chart showing when each med goes in, what to avoid, and why. This is especially helpful for older adults or people on complex regimens.
- Adjust for real life: If you miss a dose, the system doesn’t just remind you again. It recalculates based on the label’s minimum interval. "You took your amoxicillin at 2 PM. Next dose can’t be until 10 PM."
These systems use standardized medical language (RxNorm and SNOMED CT) to make sure the app understands "ibuprofen 400 mg" the same way your pharmacist does. This prevents confusion between brand and generic names.
Real People, Real Results
Users who switch from basic alarms to label-based systems report dramatic improvements. On Reddit’s r/medicationadherence, one user wrote: "I was taking my diabetes meds with my coffee - which made them less effective. The app flagged it because the label said 'take on empty stomach.' I didn’t even know that was a thing. Now I take them before I even turn on the coffee maker."A 2024 AARP survey of 3,500 adults over 65 found that 76.4% had better adherence when reminders included label-based instructions like "take with breakfast" instead of just "7 AM." Visual timelines helped them see how their meds fit into their daily routine - not just a list of times.
On Trustpilot, CareZone users gave it a 4.7/5 rating, with one comment: "It reads my prescription labels and automatically sets reminders with the correct intervals between my blood pressure meds and diabetes drugs, which my doctor said was critical but I never understood from the paper labels."
But it’s not perfect. One user on the Apple App Store wrote: "It didn’t recognize that my antibiotic needed 12-hour intervals but couldn’t be taken at 2 AM, causing me to miss doses." That’s a common flaw - some systems don’t account for sleep schedules. The best ones let you set "do not disturb" windows or adjust for personal routines.
What to Look for in a Smart Reminder App
Not all apps are built the same. Here’s what to check before you download:- Label scanning: Can it read your actual prescription label? If it only lets you type in meds manually, skip it.
- Drug interaction checker: Does it warn you if your meds clash? Look for integration with RxNorm or FDA databases.
- Food and timing rules: Can it handle "take with food," "empty stomach," or "avoid grapefruit"?
- Flexible scheduling: Can it adjust for 8-hour intervals without forcing a 2 AM alarm?
- Visual timeline: Does it show your day as a chart, not just a list of alarms?
- Pharmacist review option: The most reliable systems let you send your schedule to a pharmacist for a quick check - especially if you’re on 5+ meds.
Top choices in 2025 include Medisafe (used by over 2.5 million people), MyTherapy, and CareZone. Epic’s MyChart platform, now integrated with label interpretation, is also becoming popular for patients who get their prescriptions through large health systems.

When the Label Isn’t Clear
Not every label is perfect. A 2023 study in the Journal of the American Pharmacists Association found that 22.4% of generic drug labels use vague or non-standard language - like "take as needed" or "take twice daily" without specifying times. Some even use symbols or abbreviations that aren’t universally understood.If your label is unclear, don’t guess. Call your pharmacy. Ask: "Can you clarify the timing and food instructions for this med? I’m using a reminder app and want to make sure it’s set right."
Also, your doctor might have adjusted your dose or schedule based on your body’s response. That change might not be on the label. Always compare your app’s schedule with what your doctor told you. If they conflict, trust your doctor - but make sure the app knows about the change.
The Bigger Picture: Why This Matters
Poor medication adherence causes 1.5 million preventable injuries and deaths in the U.S. every year, according to the Institute of Medicine. Most of those aren’t from forgetting - they’re from taking the wrong dose, at the wrong time, with the wrong food, or alongside a dangerous interaction.The FDA, WHO, and CMS are now requiring digital health tools to use label information. By 2026, all Medicare-participating health systems must use reminder systems that reflect actual prescription labels. That’s because the data is clear: when reminders are built from the label, adherence jumps by 23.7%. The best systems - those that combine label reading with pharmacist review - see adherence rates above 85%.
This isn’t about tech. It’s about safety. Your label is your first line of defense. Your reminder app should be its second.
Quick Action Steps
- Take a photo of every new prescription label as soon as you get it.
- Download a reminder app that scans labels - don’t just type them in.
- Check that the app understands food, timing, and interaction rules.
- Set up a "do not disturb" window if you don’t want alarms at night.
- Ask your pharmacist to review your app’s schedule once a month - especially if you’re on 4+ meds.
- Update the app if your doctor changes your dose or schedule.
If you’re on a complex regimen, don’t rely on memory. Don’t rely on a basic alarm. Use your label - the one the pharmacist printed, the one the FDA requires - to build a reminder that works for your life, not against it.
Can I just use my phone’s alarm app for medication reminders?
You can, but it’s risky. Basic alarm apps don’t understand food requirements, minimum intervals between doses, or drug interactions. Setting an alarm for 8 AM for all your meds might cause you to take a pill on an empty stomach when it needs food, or take two drugs too close together. This increases your risk of side effects or overdose. Use a dedicated medication app that reads your prescription label.
What if my prescription label is hard to read or uses confusing language?
Call your pharmacy. Don’t guess. Ask them to explain the instructions in plain language: "What does 'take every 8 hours' mean for my schedule?" or "Should I take this with or without food?" Then update your reminder app with the correct info. About 22% of generic labels have unclear wording - it’s not just you.
Do I need to scan every new bottle, even if it’s the same medicine?
Yes. Even if it’s the same drug, the strength, manufacturer, or instructions can change. A new bottle might say "take with food" when the last one said "take on empty stomach." Always scan the current label. Apps like Medisafe and MyTherapy let you update labels easily - just take a new photo and confirm the changes.
Can these apps handle multiple medications with conflicting schedules?
Yes - that’s their main purpose. Advanced apps use databases of over 500,000 drug interactions to adjust your schedule. If you’re taking a blood thinner and an antibiotic that can’t be taken together, the app will space them out. It will also avoid giving you an alarm at 3 AM if your label says "do not take at night." Look for apps that use RxNorm and SNOMED CT standards for accuracy.
Are these apps safe and private?
Reputable apps like Medisafe, MyTherapy, and CareZone are HIPAA-compliant and encrypt your data. They don’t sell your information. Always check the app’s privacy policy before entering your meds. Avoid apps that ask for unnecessary permissions like access to your contacts or location. If the app lets you connect to your EHR (like Epic or MyChart), that’s a good sign - it means your doctor’s office is involved in keeping your data accurate.
What if my doctor changes my dose or schedule?
Update your app immediately. Even if the label hasn’t changed yet, your doctor’s instructions override the printed label. Go into the app, edit the dose or timing, and add a note like "Dr. Lee changed to 5 mg daily as of 11/10/2025." Some apps let you share your updated schedule with your pharmacist or doctor directly - use that feature.
Deepak Mishra
November 16, 2025 AT 07:00OMG I JUST REALIZED MY APP SET MY AMOXICILLIN FOR 2AM 😭 I WAS WAKING UP AT 2AM TO TAKE IT AND NOW I’M SLEEPING LIKE A BABY!! THANK YOU FOR THIS POST!! 🙏❤️
Danish dan iwan Adventure
November 18, 2025 AT 05:31Label parsing via OCR is a statistical illusion. RxNorm is proprietary garbage. Real adherence requires human pharmacists, not AI parsing corrupted PDFs from CVS.
98.7% accuracy? That’s a marketing lie. I’ve seen apps misread 'q8h' as 'twice daily.'
Oyejobi Olufemi
November 19, 2025 AT 14:40They never tell you the truth... the FDA doesn’t regulate label clarity... the pharmaceutical companies design labels to confuse you... they WANT you to mess up... so you come back for more pills... it’s a business model... it’s not about health... it’s about profit... and your app? It’s just another cog... you’re being manipulated... by the system...
And don’t even get me started on MyChart... they’re selling your data to insurers... they know when you miss doses... and they raise your premiums... you’re being watched... always...
They don’t care if you live or die... they care if your bloodwork looks good on their quarterly report...
Wake up.
Wake up.
Wake up.
Diane Tomaszewski
November 20, 2025 AT 00:23I used to just set alarms but now I scan every label and the app reminds me to wait 30 mins before coffee for my thyroid med... it’s so simple but it actually works now
I feel less stressed about it
Teresa Smith
November 21, 2025 AT 16:49The paradigm shift here is not technological-it is epistemological. We have moved from compliance as obedience to adherence as cognition.
The label is not merely an instruction-it is a covenant between patient and pharmacopeia.
To reduce it to algorithmic parsing is to reduce medicine to mechanics.
Yet, paradoxically, the very mechanism that commodifies the act of taking pills also restores agency to the patient.
This is not an app.
This is a reclamation of autonomy in a system designed to disempower.
And for that, we must be grateful-not for the technology, but for the humility it demands of us.
ZAK SCHADER
November 23, 2025 AT 14:46Why do we even need apps? Back in my day we just wrote it on a sticky note and took it when we remembered. No fancy scanning. No AI. No data mining. Just common sense.
Now everyone’s a tech bro pretending they’re saving lives with a phone app.
Pathetic.
John Mwalwala
November 24, 2025 AT 00:14Did you know that 72% of label misreads happen because the font size is too small? The FDA allows 6pt font on labels. That’s smaller than a grain of rice.
And the OCR engines? They’re trained on perfect scans from brand-name drugs. Generic labels? They’re printed on cheap ink on glossy paper that reflects light wrong.
It’s not user error-it’s design failure.
And the apps? They’re just covering up a systemic failure with a shiny UI.
Real solution? Mandate 10pt font. No apps needed.
David Rooksby
November 24, 2025 AT 07:26Look, I get it, scanning labels sounds smart, but have you ever tried scanning a label on a 50-pill bottle that’s been rattling around in your gym bag for three weeks? The ink’s smudged, half the text is gone, the barcode’s peeled off, and your phone’s camera is covered in lint.
Then you get a notification saying 'Unable to parse: unknown substance detected.'
So you manually type it in... and guess what? You misread '10 mg' as '100 mg' because you’re tired and your glasses are dirty.
And now you’ve got a new problem.
Technology doesn’t fix human error-it just adds more steps to it.
And don’t even get me started on the 12-hour interval that forces you to wake up at 3 AM because your app doesn’t know you’re a night owl.
It’s not a solution.
It’s a glorified to-do list with delusions of grandeur.
Jamie Watts
November 25, 2025 AT 17:09Everyone’s talking about apps but nobody’s talking about the real problem-your pharmacist doesn’t explain anything
You get a bottle and walk away and the label is written in lawyer language
And your doctor doesn’t have time to explain either
So you guess
And then you blame the app when it messes up
But the app is just reflecting the mess they gave you
Fix the system first
Not the app
Stop putting tech on the hook for bad communication
It’s not the scanner that’s broken
It’s the whole damn process
Daniel Stewart
November 26, 2025 AT 15:07There is a melancholy beauty in the fact that we now require artificial intelligence to interpret the very language meant to protect us from harm.
Our medications are encoded in symbols we no longer understand.
Our bodies have become systems to be calibrated by algorithms.
And yet, in this digital mediation, we find a strange intimacy-our survival now depends on a machine reading the words we cannot read ourselves.
Is this progress?
Or merely the quiet surrender of embodied knowledge to the cloud?
Rachel Wusowicz
November 27, 2025 AT 16:22EVERYTHING IS A LIE.
THE FDA? IN BED WITH PHARMA.
THE APPS? TRACKING YOUR SLEEP PATTERNS TO SELL YOU SLEEP PILLS LATER.
THE 'LABEL' IS A TRAP-THEY PRINT 'TAKE WITH FOOD' BUT THE REAL INSTRUCTIONS ARE IN THE SMALL PRINT ON THE BACK OF THE BOX THAT NO ONE READS.
THEY WANT YOU TO THINK YOU’RE IN CONTROL-BUT YOU’RE JUST A DATA POINT IN A MACHINE THAT PROFITS FROM YOUR CONFUSION.
THEY’LL NEVER CHANGE THE FONT SIZE.
THEY’LL NEVER MAKE THE LABELS CLEAR.
THEY’LL JUST KEEP SELLING YOU APPS THAT SAY THEY’RE HELPING YOU-WHILE THEY SELL YOUR MEDICATION HISTORY TO INSURANCE COMPANIES WHO RAISE YOUR RATES WHEN YOU MISS A DOSE.
YOU’RE NOT BEING HELPED.
YOU’RE BEING MONETIZED.
WAKE UP.
WAKE UP.
WAKE UP.
Dan Angles
November 28, 2025 AT 23:17As a healthcare professional, I commend the emphasis on label-based systems. However, we must not overlook the human element.
Technology augments-but does not replace-clinical dialogue.
Patients require explanation, not just automation.
App notifications are useful, but they cannot substitute for a pharmacist saying, 'This med can cause dizziness-don’t drive for the first week.'
Use the app. But also ask questions.
And if you’re unsure-call your pharmacy.
There is no algorithm that can replicate compassion.
And compassion is what keeps people alive.
Ankit Right-hand for this but 2 qty HK 21
November 30, 2025 AT 12:20This whole thing is just American nonsense.
In India we just take pills when we remember and if we get sick we go to the doctor.
No apps.
No scanning.
No overthinking.
Why do you need a machine to tell you when to take a pill?
You’re not a robot.
Stop outsourcing your brain to Silicon Valley.
Real medicine is simple.
Stop making it complicated.
And stop pretending your phone is your doctor.