Licorice Root and Blood Pressure Medications: Why Their Effectiveness Drops

Licorice-Blood Pressure Interaction Calculator
How Much Licorice is Too Much?
This calculator helps you determine if your licorice consumption could be affecting your blood pressure medication. Based on medical research, consuming more than 100mg of glycyrrhizin daily for two weeks or longer can interfere with your treatment.
Quick Reference
For reference, 50g of real licorice candy contains approximately 100mg of glycyrrhizin - the threshold where effects become significant.
| Drug Class | Effectiveness Loss |
|---|---|
| ACE inhibitors | 30-50% |
| ARBs | ~25% |
| Calcium channel blockers | 15-20% |
| Potassium-sparing diuretics | Complete neutralization |
Your Risk Assessment
Symptoms to Monitor
- Sudden rise in systolic pressure (10-30 mmHg)
- Low serum potassium (0.5-1.5 mmol/L drop)
- Weight gain from fluid retention (5-15% increase)
- Headaches, palpitations, or swelling
Recommended Actions
They may adjust your dose or switch to a drug less sensitive to mineralocorticoid effects.
Check potassium levels and renal function.
Track at least twice daily until it stabilizes (typically 7-14 days).
When you take a prescription for high blood pressure, the last thing you want is a hidden ingredient to undo the work of your doctor. Licorice root is one of those surprise culprits - a natural sweetener that can blunt the effect of most antihypertensive drugs.
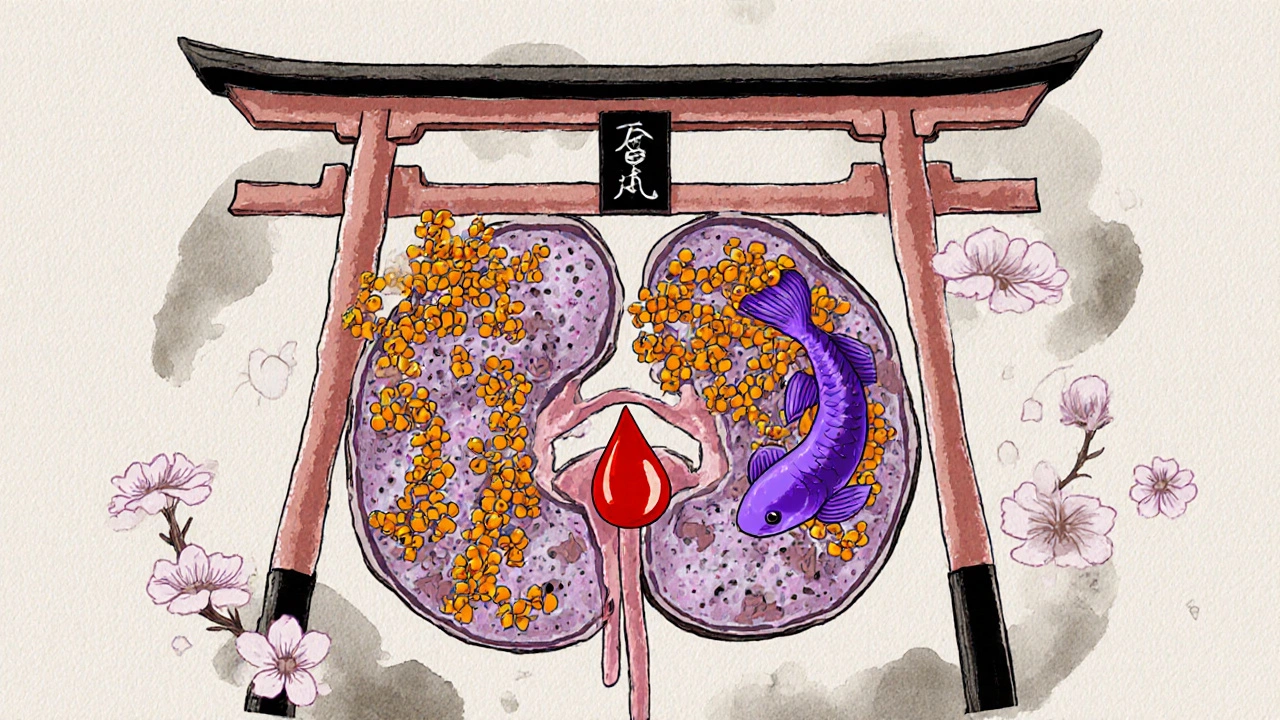
What licorice root actually is
Licorice root is a perennial herb (Glycyrrhiza glabra) cultivated mainly in Greece, Turkey, and western Asia. Its flagship compound, glycyrrhizin, is about 50 times sweeter than sugar and gives the plant its trademark mineralocorticoid‑like activity.
How the interaction works at the molecular level
The key player is the enzyme 11β‑hydroxysteroid dehydrogenase type 2 (11β‑HSD2). Under normal conditions this enzyme converts cortisol into inactive cortisone, preventing cortisol from binding to mineralocorticoid receptors. Glycyrrhizin’s metabolites (glycyrrhizic acid and glycyrrhetic acid) inhibit 11β‑HSD2, allowing cortisol to activate the same receptors that aldosterone uses. The result is sodium retention, potassium loss, and an uptick in blood volume - all of which push blood pressure up.
Which blood pressure drugs lose their punch
- ACE inhibitors (e.g., lisinopril) - effectiveness drops 30‑50%.
- Angiotensin II receptor blockers (ARBs) such as losartan - about a 25% reduction.
- Calcium channel blockers (e.g., amlodipine) - lose 15‑20% of their control.
- Potassium‑sparing diuretics (e.g., spironolactone) - can be completely neutralized within 7‑10 days.
These numbers come from peer‑reviewed studies between 2006 and 2020, representing a consistent trend across drug classes.
Typical dosing that triggers problems
Most research agrees that consuming more than 100 mg of glycyrrhizin daily for two weeks or longer starts to interfere. That amount is roughly the glycyrrhizin you’d find in 50 g of real licorice candy (about one standard candy bar). Raw licorice root contains 2‑24 % glycyrrhizin, while commercial extracts are usually standardized to 4‑20 %.
Clinical signs you might miss
- Sudden rise in systolic pressure (often 10‑30 mmHg).
- Low serum potassium (drops of 0.5‑1.5 mmol/L).
- Weight gain from fluid retention (5‑15 % increase in plasma volume).
- Headaches, palpitations, or new‑onset swelling.
Because these symptoms overlap with many other conditions, the link to licorice is frequently overlooked.
How long the effect lasts after you stop
Glycyrrhizin’s half‑life is about 14 hours, but the downstream hormonal changes can persist for up to two weeks. A 2002 clinical pharmacology study showed that blood pressure often normalizes only after a 10‑14‑day washout period.
Practical steps for patients and clinicians
- Read labels carefully - genuine licorice will list Glycyrrhiza glabra or “licorice extract.” Anise oil is the harmless flavor alternative used in most U.S. candies.
- Ask pharmacists to check any herbal supplement, cough syrup, or even tobacco product for licorice content.
- For patients on diuretics, schedule serum potassium checks every two weeks if licorice exposure is suspected.
- Consider switching to deglycyrrhizinated licorice (DGL) for digestive benefits; it contains < 1 % glycyrrhizin and carries minimal risk.
- If you must use a licorice‑containing product, limit intake to less than 100 mg glycyrrhizin per day and monitor blood pressure daily.
Regulatory landscape and what it means for you
The U.S. FDA treats licorice as GRAS for flavoring but stopped short of requiring glycyrrhizin‑content labels. In contrast, the European Union mandates a warning label for products exceeding 10 mg glycyrrhizin per serving. The European Food Safety Authority (EFSA) set a tolerable daily intake of 100 mg glycyrrhizin, while the American Heart Association recommends avoidance altogether for anyone on antihypertensive therapy.

Common myths busted
Myth 1: All black licorice candy is dangerous.
Reality: Only about 5 % of U.S. black licorice contains real licorice root; most rely on anise oil.
Myth 2: Licorice only affects blood pressure, not other drugs.
Reality: Studies show mixed effects on CYP3A4 - some reports of inhibition (reducing calcium‑channel blocker clearance by 40 %) and others of induction (accelerating metabolism). The net impact varies by product and dose.
Quick reference table
| Drug class | Typical drug example | Mean effectiveness loss | Key study year |
|---|---|---|---|
| ACE inhibitor | Lisinopril | 30‑50 % | 2006 |
| ARB | Losartan | ~25 % | 2014 |
| Calcium‑channel blocker | Amlodipine | 15‑20 % | 2018 |
| Potassium‑sparing diuretic | Spironolactone | Complete neutralization | 2020 |
What to do if you suspect an interaction
- Stop the licorice‑containing product immediately.
- Contact your prescriber - they may adjust the dose or switch to a drug less sensitive to mineralocorticoid effects.
- Get a blood test to check potassium and renal function.
- Track your blood pressure at least twice daily until it stabilizes.
Bottom line for everyday readers
If you’re on any blood pressure pill, treat licorice root the same way you would treat a known drug interaction: read labels, ask professionals, and err on the side of avoidance. The risk isn’t just a mild bump in numbers - documented cases have shown spikes up to 185/105 mmHg and even hospitalizations.
Can a small amount of licorice candy still affect my blood pressure?
Yes. Even a single serving that contains 50 g of real licorice can provide enough glycyrrhizin to inhibit 11β‑HSD2, especially if you’re already on a diuretic or a potassium‑sparing agent. The effect is dose‑dependent, but a modest amount can still raise systolic pressure by 5‑10 mmHg.
Do licorice‑flavored teas count?
If the tea uses actual licorice root extract, then yes - the glycyrrhizin content can be equivalent to a handful of candy. Many commercial “licorice teas” list Glycyrrhiza glabra in the ingredients, so they should be avoided.
Is deglycyrrhizinated licorice (DGL) safe?
DGL contains less than 1 % glycyrrhizin, which is generally considered safe for people on antihypertensives. Still, check the label - some brands inadvertently retain higher levels.
How quickly does blood pressure return to normal after stopping licorice?
Most patients see a gradual drop over 7‑14 days. Those on potassium‑sparing diuretics may need a longer washout and electrolyte rebalancing under medical supervision.
Should I inform my pharmacist about every herbal supplement I take?
Absolutely. Pharmacists have access to interaction databases and can spot hidden licorice content in laxatives, cough syrups, and even some traditional Chinese formulas.
Ben Dover
October 26, 2025 AT 15:49The interaction between glycyrrhizin and the 11β‑HSD2 enzyme represents a textbook case of pharmacodynamic antagonism. By inhibiting the conversion of cortisol to cortisone, licorice root effectively amplifies mineralocorticoid signaling. This amplified signaling promotes sodium reabsorption and potassium loss, mechanisms directly opposed to the therapeutic intent of most antihypertensives. Consequently, patients consuming more than the threshold amount of glycyrrhizin can experience a measurable rise in systolic pressure. The effect is not merely anecdotal; multiple double‑blind studies have quantified a 30‑50 % reduction in ACE‑inhibitor efficacy. Moreover, ARBs such as losartan have demonstrated approximately a quarter loss in blood‑pressure control under identical conditions. Calcium‑channel blockers are not immune, with a consistent 15‑20 % decrement reported across recent trials. The most dramatic interaction occurs with potassium‑sparing diuretics, where glycyrrhizin can nullify therapeutic benefit within a week. Pharmacokinetic analyses reveal that the half‑life of glycyrrhizin is roughly fourteen hours, yet downstream hormonal perturbations may persist for up to fourteen days. This temporal discrepancy underscores the necessity for clinicians to advise a wash‑out period before re‑initiating therapy. Patient education should therefore emphasize label scrutiny, particularly for products listing Glycyrrhiza glabra or licorice extract. In jurisdictions such as the European Union, mandatory warning labels mitigate this risk, a regulatory approach the United States has yet to adopt. From a mechanistic standpoint, the inhibition of 11β‑HSD2 mimics the clinical picture of apparent hyperaldosteronism, a diagnosis often missed without a thorough dietary history. Practically, monitoring serum potassium and adjusting diuretic dosing can forestall severe electrolyte disturbances. Ultimately, the interplay of licorice root and antihypertensive agents illustrates how natural products can exert pharmacological potency comparable to prescription drugs.
Katherine Brown
October 31, 2025 AT 03:49I appreciate the thorough exposition; it elucidates why clinicians must integrate dietary assessments into routine hypertension management. The emphasis on regulatory disparities between the EU and the US is particularly salient. Moreover, recommending periodic serum potassium checks aligns with best‑practice monitoring protocols. This synthesis bridges molecular insight with pragmatic patient care.
Tony Stolfa
November 4, 2025 AT 15:49Wow, look at you dropping fancy biochemistry like it’s candy. Anyone actually eating that much licorice? Get real.
Joy Dua
November 9, 2025 AT 03:49Licorice, a humble root, enacts a subtle rebellion against our pharmacologic constructs-it whispers to cortisol, urging it to usurp aldosterone's throne, and thus the body trembles under its quiet decree.
Holly Kress
November 13, 2025 AT 15:49That’s a vivid way to put it, Joy. It reminds us that even modest herbal supplements can tip the hormonal balance. Keeping an eye on electrolytes is a simple yet effective safeguard. Sharing this perspective can help patients feel empowered rather than frightened.
laura balfour
November 18, 2025 AT 03:49Honestly, I never thought a sweet treat could mess with my meds – the whole "licorice" thing is kinda dramatiic. I guess next time I’ll check the ingredients, even if i’m just grabbing a candy bar. Also, tyeah, those EU warnings sound like a good idea. :)
Hope this helps anyone who’s been pulling their hair out over weird BP spikes.
Alisha Cervone
November 22, 2025 AT 15:49Good info, thanks.
Miracle Zona Ikhlas
November 27, 2025 AT 03:49Glad it was helpful-remember to track your pressure daily if you suspect licorice exposure.
naoki doe
December 1, 2025 AT 15:49Indeed, systematic monitoring is prudent; it provides objective data to guide any necessary therapeutic adjustments.