Melanoma Stages Explained: Complete Guide to Diagnosis & Treatment
Melanoma Staging Calculator
Determine Your Melanoma Stage
This calculator uses the AJCC 8th edition staging system to help determine melanoma stage based on key clinical parameters.
Stage
This stage indicates
Typical Treatment Options
The term Melanoma is a type of skin cancer that originates from pigment‑producing cells called melanocytes and is the most aggressive form of skin cancer. Understanding the different melanoma stages can feel overwhelming, but breaking them down into clear, bite‑size pieces makes the journey easier. This guide walks you through every stage, why staging matters, the key factors doctors look at, and what treatment options typically line up with each level of disease.
What Is Melanoma and How Does It Differ From Other Skin Cancers?
Skin cancer covers a group of cancers that start in the skin, including basal cell carcinoma, squamous cell carcinoma, and melanoma. While basal and squamous cell cancers rarely spread, melanoma has a high chance of metastasizing if not caught early. That’s why doctors rely on precise staging to decide how aggressively to treat the disease.
Why Staging Matters
Staging tells you three things at once: how far the tumor has grown, whether it has reached lymph nodes or distant organs, and what the likely prognosis is. A clear stage helps clinicians choose the most effective therapy, predicts survival odds, and guides follow‑up schedules. In short, the stage is the roadmap for both patients and doctors.
Overview of the Staging Systems Used for Melanoma
The most widely accepted system is the American Joint Committee on Cancer (AJCC) staging system, currently in its 8th edition. It combines tumor thickness, ulceration, nodal involvement, and metastasis into a numeric stage from 0 to IV. While older systems like the Clark level are still referenced, the AJCC framework provides the most detailed prognostic information.
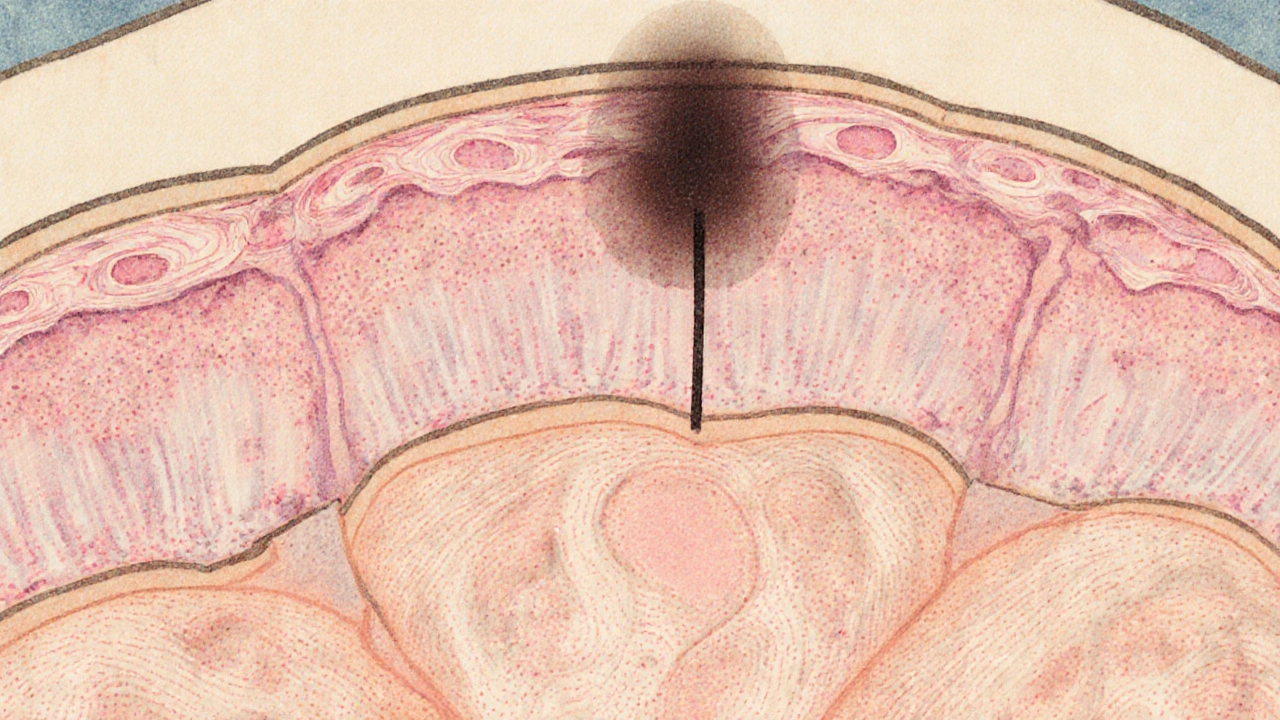
Stage 0 - Melanoma In Situ
At this earliest point, cancer cells are confined to the epidermis and have not invaded deeper layers. Under a microscope, pathologists often describe it as "melanoma in situ. No lymph node testing is needed, and surgical excision with narrow margins typically cures the disease.
Stage I - Thin, Localized Melanoma
Stage I tumors have breached the epidermis but remain relatively thin. The AJCC divides this stage into IA and IB based on two main metrics:
- Breslow thickness - measured in millimeters from the top of the skin to the deepest tumor cell.
- Ulceration - whether the tumor surface is broken.
Stage IA usually means a thickness ≤1.0 mm without ulceration, while IB involves thickness up to 2.0 mm or the presence of ulceration. Wide local excision with 1‑2 cm margins is the standard, and sentinel lymph node biopsy (SLNB) may be considered for thicker lesions.
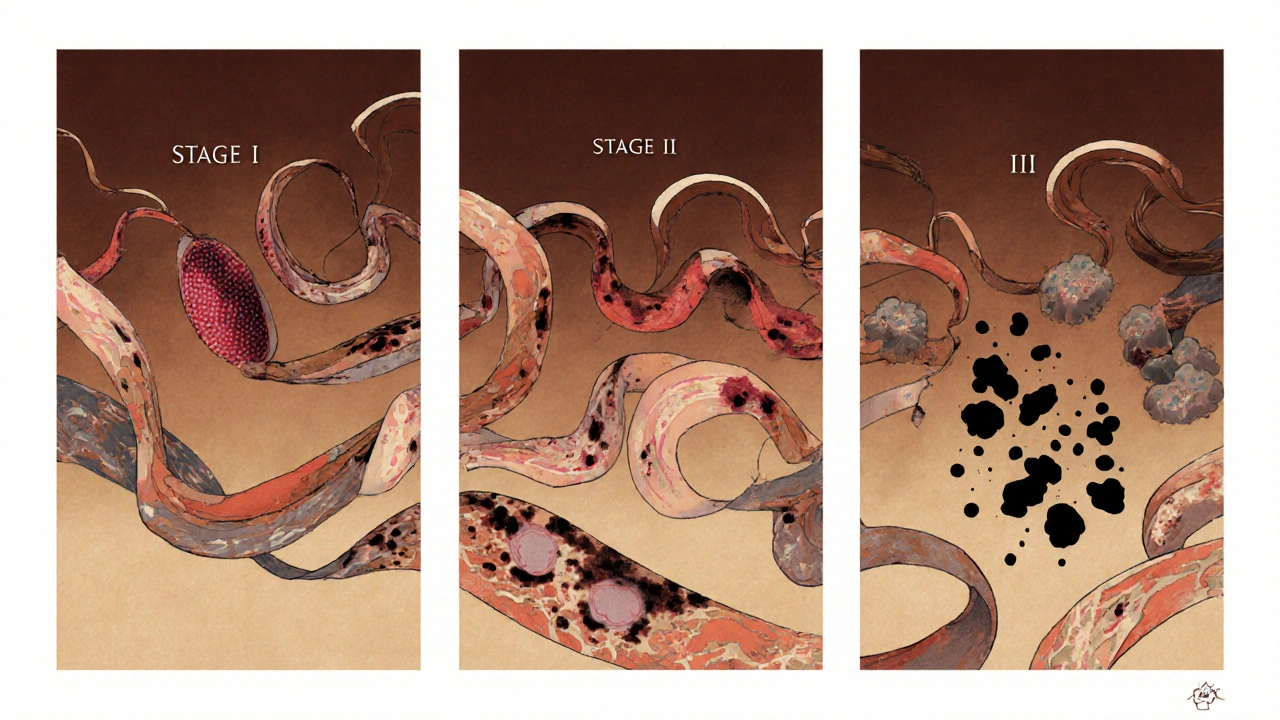
Stage II - Thick, Still Localized
Stage II cancers are thicker (over 2.0 mm) but still haven’t reached lymph nodes. Subcategories IIA, IIB, and IIC depend on exact thickness, ulceration, and mitotic rate. The risk of spread grows sharply as thickness increases.
Besides surgery, clinicians often discuss adjuvant therapy-such as immune checkpoint inhibitors (e.g., pembrolizumab) or targeted agents (e.g., BRAF/MEK inhibitors)-especially for high‑risk IIC tumors.
Stage III - Regional Spread to Lymph Nodes
When melanoma cells reach nearby lymph nodes, the disease moves into Stage III. The AJCC further splits this into IIIA‑IIID based on:
- Number of positive nodes.
- Size of nodal metastases.
- Presence of in‑transit metastases (tumor deposits between the primary site and nodal basin).
Management usually combines surgical removal of affected nodes, followed by systemic adjuvant therapy. Clinical trials have shown that immunotherapy dramatically improves recurrence‑free survival in this group.
Stage IV - Distant Metastasis
Stage IV indicates that melanoma has spread to distant organs such as the lungs, liver, brain, or bone. Prognosis varies widely depending on the organ involved and the specific genetic mutations of the tumor.
First‑line treatment often involves combination immunotherapy (e.g., nivolumab + ipilimumab) or targeted therapy if the tumor carries a BRAF V600 mutation. Radiation or surgery may be used for isolated brain lesions, but systemic therapy remains the cornerstone.
Key Factors That Influence Staging Details
Beyond the basic thickness and ulceration, several pathological features help clinicians fine‑tune the stage:
- Breslow thickness measures depth in mm and is the strongest predictor of survival.
- Clark level describes which skin layer the tumor has invaded (used less often now but still referenced).
- Ulceration presence signals a higher risk of spread.
- Sentinel lymph node biopsy detects microscopic nodal involvement, guiding stage III classification.
- Mitotic rate - how quickly tumor cells are dividing, expressed as mitoses per mm².

Treatment Options by Stage
Each stage has a typical treatment pathway, though personal health, tumor genetics, and patient preference can shift the plan.
- Stage 0‑I: Surgical excision alone, with margins ranging from 0.5 cm (in‑situ) to 2 cm (thin invasive).
- Stage II: Wide excision plus consideration of adjuvant immunotherapy (e.g., pembrolizumab) for high‑risk tumors.
- Stage III: Complete lymph node dissection when indicated, followed by adjuvant immunotherapy or BRAF/MEK targeted therapy if a BRAF mutation is present.
- Stage IV: Systemic therapy is primary. Immunotherapy includes checkpoint inhibitors that unleash the immune system against melanoma has become the standard, with targeted therapy reserved for BRAF‑mutated disease.
Follow‑Up and Prognosis
Even after successful treatment, melanoma demands lifelong surveillance. Typical follow‑up schedules are:
- Every 3‑6 months for the first 2 years.
- Every 6‑12 months through year 5.
- Annual skin exams thereafter.
Dermoscopic skin checks and patient‑self‑exams are essential. Blood work and imaging (CT, PET, MRI) are reserved for higher stages or suspicious symptoms.
Quick Reference Table: Stages at a Glance
| Stage | Depth (Breslow) | Ulceration | Node Involvement | Typical Treatment |
|---|---|---|---|---|
| 0 (In situ) | - | Absent | None | Excision only |
| IA | ≤1.0 mm | Absent | None | Wide excision ± SLNB |
| IB | ≤2.0 mm or ulcerated ≤1.0 mm | Present/Absent | None | Wide excision ± SLNB |
| IIA-IIC | >2.0 mm | Variable | None | Excision + adjuvant therapy (high‑risk) |
| IIIA-IIID | Any | Variable | Positive nodes or in‑transit | Node dissection + systemic adjuvant |
| IV | Any | Variable | Distant organs | Systemic immunotherapy / targeted therapy |
Frequently Asked Questions
Can a thin melanoma still be dangerous?
Yes. Even melanomas thinner than 1 mm can ulcerate or have a high mitotic rate, both of which raise the risk of spread. That’s why a pathology report looks at multiple factors, not just thickness.
What does a sentinel lymph node biopsy involve?
A tiny amount of radioactive dye and/or blue dye is injected near the tumor. The surgeon then tracks the first draining lymph node (the “sentinel”) and removes it for pathological analysis. If cancer cells are found, further node removal may be recommended.
Are there lifestyle steps that can lower my risk of melanoma?
Yes. Regular sunscreen use (SPF 30+), wearing protective clothing, avoiding peak UV hours, and conducting monthly skin self‑exams are proven measures. For those with a strong family history, regular dermatologist visits are advisable.
How effective are immunotherapy drugs for advanced melanoma?
Checkpoint inhibitors like pembrolizumab and nivolumab have produced 5‑year overall survival rates above 30% for stage IV patients, a dramatic improvement over chemotherapy’s < 10% rates.
When should I see a doctor about a new mole?
If a mole changes in size, shape, color, or starts itching or bleeding, schedule an appointment right away. Using the ABCDE rule (Asymmetry, Border, Color, Diameter, Evolving) is a quick self‑check.
Rachel Valderrama
October 21, 2025 AT 15:21Congrats on mastering something you could've Googled in five seconds.
Brandy Eichberger
October 29, 2025 AT 17:06Ah, the elegance of a well‑structured staging system-truly the haute couture of oncologic taxonomy. While the average reader might skim over Breslow thickness and ulceration, these nuances separate a casual observation from a scholarly discourse. The AJCC 8th edition, with its granular sub‑categories, offers clinicians a roadmap that feels almost poetic in its precision. One cannot help but admire how each millimeter of depth translates into a cascade of therapeutic decisions. So, dear seekers of clarity, cherish these details; they are the very scaffolding upon which life‑saving interventions are built.
Eli Soler Caralt
November 6, 2025 AT 19:50i cant help but feel that the very act of categorizing life into stages is a modern echo of ancient mysticism 🌌. the skin, that humble canvas, becomes a ledger of our mortality - each ulcer, each mitotic whisper a line in an ever‑evolving poem. btw, the AJCC system? kinda like a cosmic spreadsheet, lol. misspelling is just art, n\'t the end 🧐. 🚀
Eryn Wells
November 14, 2025 AT 22:33Thank you for breaking down the technical jargon into something we can all grasp! 🌟 Remember, early detection and regular skin checks are key, no matter where you live. A friendly reminder to share this knowledge with friends and family-knowledge is the best sunscreen! 😊
Kathrynne Krause
November 23, 2025 AT 01:16Alright, team, let’s pump up the volume on prevention! 🎉 Sunscreen isn’t just a beach‑day accessory; it’s a daily armor against those sneaky UV ninjas. Pair that with a habit of monthly self‑checks, and you’re basically giving melanoma the boot. Keep those margins wide, keep the margins clean, and never underestimate the power of a well‑timed dermatologist visit. You’ve got this-let’s turn knowledge into action!
Chirag Muthoo
December 1, 2025 AT 04:00It is advisable to follow the recommended follow‑up schedule delineated in the guideline, namely three to six‑month intervals for the initial two years, followed by biannual examinations up to the fifth year, and annual reviews thereafter. Adherence to these intervals facilitates early identification of recurrence and enhances overall prognosis.
Angela Koulouris
December 9, 2025 AT 06:43Great overview! Remember, when you’re walking a patient through their treatment plan, framing each step as a victory can boost morale. Celebrate the margins you achieve during excision, and keep the conversation lively yet respectful.
erica fenty
December 17, 2025 AT 09:26Key point: staging informs therapeutic algorithm; therefore, accurate pathological reporting is non‑negotiable. Also, sentinel node biopsy (SLNB) > 0.8 mm thickness? ✅. Adjuvant immunotherapy improves recurrence‑free survival-data from CheckMate‑067 supports this. Proper surveillance protocol mitigates late‑stage presentation.
Jasmina Redzepovic
December 25, 2025 AT 12:10Listen, the U.S. leads in melanoma research, and we should be proud of the breakthroughs we’ve achieved. Any talk about “global guidelines” that downplay American standards borders on naive. Our clinicians don’t need foreign advice when we’ve got the FDA, NCCN, and world‑class trials right at home.
Erika Thonn
January 1, 2026 AT 13:53i think the whole thing about "staging" is kind of like trying to put a wild river in a glass bottle, you know? you can measure the depth of a river with a ruler, but you cant capture the flow, the energy, the hidden currents that push it forward. the same way, when doctors look at breslow thickness and ulceration, they are looking at the surface of a deep story. each mitosis is like a tiny rebel pushing back against the body's order, and each ulcerated spot is a scar of battle won or lost. sometimes i wonder if the ink on the pathology report ever feels the weight of the patient’s hopes. the oncology community tries to codify everything: i, ii, iii, iv, and then the sub‑categories that sound like a math class. but behind each number is a human being, a mother, a student, a dreamer. why do we reduce them to roman numerals? why do we love to talk about "five‑year survival" like it's a scoreboard? it's a reminder that numbers are cold, but the lives they represent are warm. i read about immunotherapy and it's like a sci‑fi movie-nivolumab and ipilimumab teaming up like superheroes. yet, the side effects can be a nightmare, a reminder that even the best weapons have collateral damage. the brain metastases? that’s a whole different battlefield. the radiation? it's a precise sniper. all of this, wrapped up in a table, a quick reference. but you can't see the sweat in the surgeon's gloves, the late‑night calls, the whispered prayers. i think the best thing we can do is to remember that the staging guide is a map, not the territory. if we stay humble, if we keep learning, if we keep listening, then maybe, just maybe, we can make each stage a little less scary. and maybe, someday, we won't need to stage at all because the disease will be a thing of the past.