Oral Chemotherapy: How to Stay on Track, Stay Safe, and Manage Side Effects

More than half of all new cancer drugs approved since 2018 come in pill or liquid form you can take at home. Oral chemotherapy is no longer the exception-it’s the norm. For many patients, it means fewer clinic visits, less time away from work, and more control over their daily routine. But this convenience comes with a hidden cost: oral chemotherapy demands far more from you than just swallowing a pill. If you miss a dose, take it with the wrong food, or don’t recognize early warning signs, the treatment can fail-or worse, become dangerous.
How Oral Chemotherapy Works (And Why It’s Different)
Oral chemotherapy drugs attack cancer cells the same way IV chemo does: by disrupting cell division, damaging DNA, or blocking the signals that let tumors grow. But the delivery method changes everything. Instead of a nurse injecting drugs into your vein, you’re responsible for taking the right dose, at the right time, every single day. That’s why the same drug can work perfectly in the clinic but fail at home. There are four main types of oral chemo drugs, each with unique behaviors:- Alkylating agents like cyclophosphamide damage DNA directly. They’re used for lymphoma and breast cancer, and cause hair loss, nausea, and low blood counts in over 60% of patients.
- Antimetabolites like capecitabine trick cancer cells into using fake building blocks. This leads to hand-foot syndrome-red, peeling skin on palms and soles-in more than half of users.
- Topoisomerase inhibitors like topotecan block enzymes needed for DNA replication. They’re often used in lung and ovarian cancer.
- Mitotic inhibitors like vinca alkaloids stop cells from splitting. These are less common orally but still used in some leukemia and lymphoma cases.
The Biggest Risk: Missing a Dose
Studies show only about 60% of patients take their oral chemo exactly as prescribed. That’s not laziness-it’s complexity. Some regimens require taking pills twice a day for two weeks, then stopping for a week. Others must be taken on an empty stomach, with no food for two hours before and after. One missed dose might seem small, but in cancer treatment, consistency is everything. Think of it like this: if you’re supposed to take 14 doses over 21 days, missing three doses means you’ve only received 79% of your planned treatment. That’s not a minor slip-it’s enough to let cancer cells recover and grow stronger. A 2022 study found patients with poor adherence had a 40% higher risk of disease progression compared to those who stuck to their schedule. The problem isn’t just forgetting. It’s also misunderstanding. Patients often skip doses because they feel sick, assume the drug isn’t working, or don’t realize a side effect is serious. Others double up after missing a dose, which can lead to overdose. That’s why education isn’t optional-it’s life-saving.Safety: What You Can’t Afford to Ignore
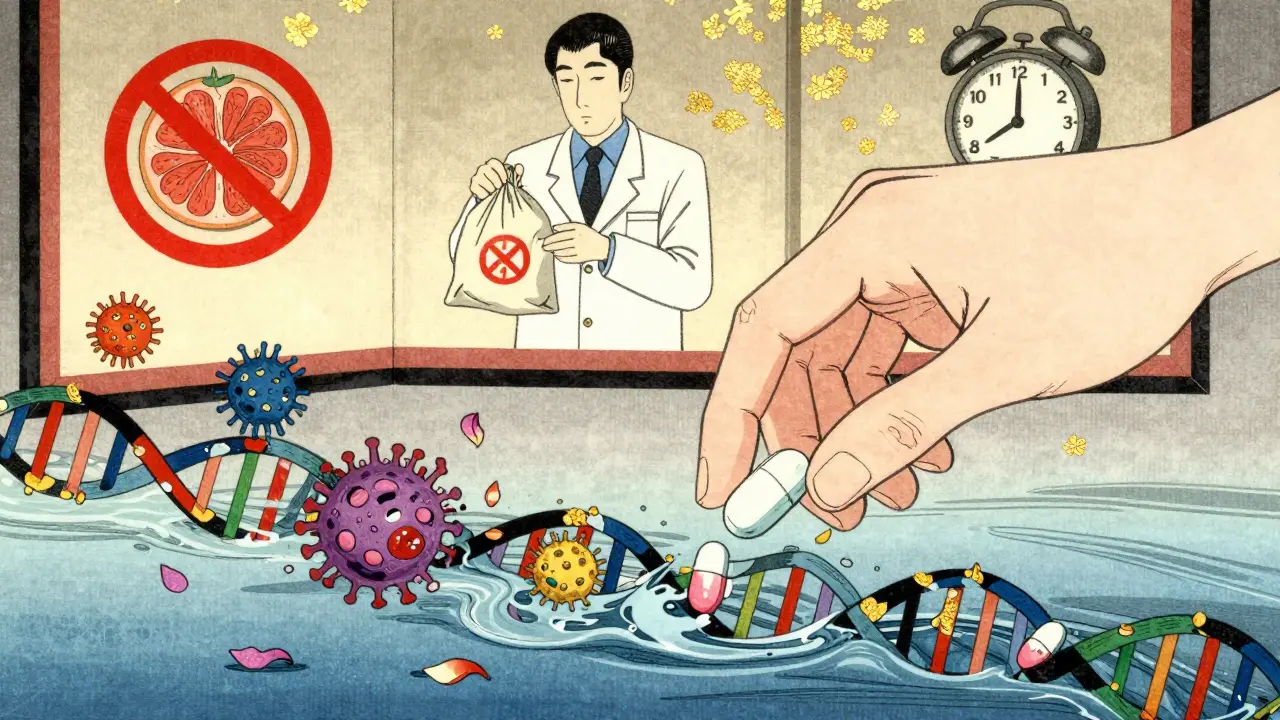
Oral chemo isn’t like a painkiller you can stash in a medicine cabinet. Many of these drugs are toxic enough to harm others if they come into contact with them. That’s why storage and disposal matter.- Storage: Most oral chemo drugs should be kept at room temperature (20-25°C), away from moisture and sunlight. Never store them in the bathroom or near the kitchen sink.
- Handling: Always wear gloves when touching pills or opening capsules. Wash your hands before and after. Pregnant people or those with weakened immune systems should avoid handling the medication.
- Disposal: Never flush pills down the toilet or throw them in the trash. Use FDA-approved medication disposal bags-these neutralize the drug and prevent environmental contamination. Most pharmacies provide them for free.
- Antacids and proton pump inhibitors (like omeprazole) can cut absorption of capecitabine by up to 50% if taken too close to the dose.
- Rifampin (used for TB) can drop dasatinib levels by 80%, making the drug useless.
- Ketoconazole (an antifungal) can spike lapatinib levels by over 300%, leading to dangerous toxicity.
Side Effects: What to Watch For
Side effects from oral chemo aren’t always obvious. Some come on slowly. Others hit hard within days. Here’s what to expect based on the drug type:- Myelosuppression: Low blood counts are common with almost all oral chemo. Watch for fatigue, dizziness, easy bruising, or frequent infections. Some drugs-like lenalidomide or dasatinib-require weekly blood tests for the first month.
- Hand-foot syndrome: Capecitabine and capecitabine-based regimens cause redness, swelling, peeling, or pain on hands and feet. If it starts, don’t wait. Use moisturizers, avoid heat, and call your care team. Left untreated, it can force you to stop treatment.
- Diarrhea and mucositis: Capecitabine and 5-FU analogs often cause watery stools or mouth sores. Don’t treat diarrhea with Imodium without checking with your doctor first-it can trap toxins in your gut.
- Liver stress: Elevated liver enzymes show up in blood tests before you feel symptoms. If your doctor orders a liver function test, don’t skip it. A 2023 study found 22% of patients on targeted oral chemo had abnormal liver values within six weeks.
- High blood pressure: Common with VEGF inhibitors like sunitinib. Check your BP at home weekly. If it’s over 140/90, contact your oncologist.
- Skin rashes: EGFR inhibitors like erlotinib cause acne-like breakouts in 80% of users. Don’t ignore them-early treatment prevents scarring and infection.
How to Stay Adherent: A Real-World Plan
You don’t have to rely on memory or willpower. Here’s what actually works, based on data from cancer centers across North America:- Use a pill organizer with time slots: Not just “morning” and “night”-use ones labeled with days of the week and times (e.g., “Day 1, 8 AM,” “Day 1, 8 PM”).
- Set two alarms: One for the dose, one as a backup 30 minutes later. Label them: “Chemo Dose - DO NOT SKIP.”
- Keep a written log: Write down each dose taken, the time, and any side effects. Use a notebook or a free app like MyTherapy or Medisafe.
- Have a backup plan: If you’re traveling, ask your pharmacy for a travel pack with extra pills. Never rely on getting a refill on the road.
- Call your team before you skip: If you’re too sick to take a dose, call your nurse or pharmacist-not your family member, not Google. They can tell you if it’s safe to skip, delay, or double up.

What Your Care Team Should Be Doing
You shouldn’t be expected to figure this out alone. The National Comprehensive Cancer Network now requires all accredited cancer centers to have a formal oral chemotherapy program. That means:- At least 45 minutes of face-to-face education when you start treatment.
- Written instructions in plain language-not medical jargon-with pictures.
- A follow-up call on day 3, day 7, and day 14 to check how you’re doing.
- Pharmacy refill tracking to spot missed doses before they become a crisis.
- Access to a 24/7 nurse line for urgent questions.
What’s Next: Smart Pills and Personalized Dosing
The future of oral chemo is already here. In 2021, the FDA approved the Proteus Discover system-a pill with a tiny sensor that sends a signal to a patch on your skin when swallowed. Your care team gets an alert if you miss a dose. It’s not perfect, but it’s a start. Another breakthrough: pharmacogenomic testing. Before you take fluoropyrimidines like capecitabine, you can now get tested for DPYD gene mutations. If you have them, you’re at high risk for life-threatening toxicity. Testing reduces severe side effects by 72%. It’s not offered everywhere yet-but if you’re starting oral chemo, ask if it’s an option. Smart pill bottles with Bluetooth are in phase 3 trials. They track when you open the bottle, and if you haven’t taken your dose after 12 hours, they text your nurse. Early results show 92% accuracy in predicting adherence. These aren’t sci-fi gadgets-they’re tools to keep you alive. And they’re only useful if you’re engaged.Can I crush or split my oral chemotherapy pills?
Never crush, split, or open capsules unless your oncologist or pharmacist specifically says it’s safe. Many oral chemo drugs are designed with special coatings to control how they’re absorbed. Crushing them can change the dose, cause dangerous spikes in drug levels, or expose you to toxic dust. If swallowing pills is hard, ask your care team about liquid versions or alternative formulations.
How do I know if my oral chemo is working?
You won’t feel it working the way you might expect. Unlike IV chemo, there’s no immediate nausea or fatigue to signal it’s active. Effectiveness is measured through blood tests, imaging scans, and tumor markers-not how you feel. Stick to your schedule and attend all follow-up appointments. Missing doses makes it impossible to tell if the drug is working or if your cancer is progressing.
Is oral chemotherapy cheaper than IV chemo?
It’s not always. While you save on clinic visits and transportation, oral chemo drugs are often significantly more expensive per dose. Insurance coverage varies widely. Some plans require prior authorization or step therapy. Always check your copay and ask your pharmacy about patient assistance programs. Many drug manufacturers offer co-pay cards or free medication programs for eligible patients.
What should I do if I accidentally take a double dose?
Call your oncology team immediately. Do not wait for symptoms. A double dose can cause severe toxicity-low blood counts, organ damage, or even hospitalization. Keep the phone number for your nurse line on your fridge or phone home screen. If you can’t reach them, go to the nearest emergency room and bring your medication bottle with you.
Can I drink alcohol while on oral chemotherapy?
It depends on the drug. Alcohol can increase liver stress, worsen dehydration from diarrhea, and interact dangerously with some chemo agents. For example, combining alcohol with metronidazole (sometimes used with oral chemo) can cause severe nausea and high blood pressure. Always ask your care team before drinking-even one glass of wine. Many oncologists recommend complete abstinence during treatment.
Should I avoid certain foods while on oral chemotherapy?
Yes. Grapefruit and Seville oranges can interfere with how your body breaks down many oral chemo drugs, raising drug levels to dangerous levels. Avoid them completely. Some drugs require an empty stomach-no food for two hours before and after. Others need to be taken with food to reduce nausea. Your care team will give you specific instructions based on your drug. Never assume-always confirm.