Physical Dependence vs Addiction: Clear Differences in Opioid Use Disorder

When someone takes opioids for chronic pain, they might start feeling sick if they miss a dose. Their stomach churns, they sweat, their muscles ache. Many assume this means they’re addicted. But that’s not true. This confusion is common-and dangerous. It leads people to stop needed medication out of fear, or worse, to dismiss real addiction because they don’t see the classic signs. Understanding the difference between physical dependence and addiction isn’t just academic. It’s life-saving.
What Physical Dependence Actually Means
Physical dependence is a normal, predictable response to taking opioids over time. Your body adapts. It’s like getting used to a new routine. If you take opioids daily for more than a week, especially at doses above 30 morphine milligram equivalents (MME) per day, your brain changes how it handles signals. Specifically, the locus coeruleus-a region that controls stress and arousal-starts producing more norepinephrine to balance the drug’s effects. When you stop taking the drug, that extra activity isn’t turned off right away. That’s when withdrawal kicks in.Withdrawal symptoms are real and uncomfortable: nausea (happens in 92% of cases), vomiting (85%), diarrhea (68%), sweating (78%), anxiety (89%), and even excessive yawning (76%). These aren’t signs of craving or loss of control. They’re biological side effects of your nervous system readjusting. You don’t need to be addicted to experience them. In fact, nearly 100% of patients on long-term opioid therapy develop this kind of dependence. That’s not a failure. It’s physiology.
Many people also develop tolerance. This means the same dose doesn’t help with pain like it used to. You might need more to get the same relief. That’s not addiction either. It’s your body adapting to the drug’s presence. Tolerance can increase by 30-50% over weeks of use. But if you’re still taking your pills as prescribed, managing pain, and not chasing the drug for euphoria or escape, you’re not addicted. You’re physically dependent.
What Addiction Really Looks Like
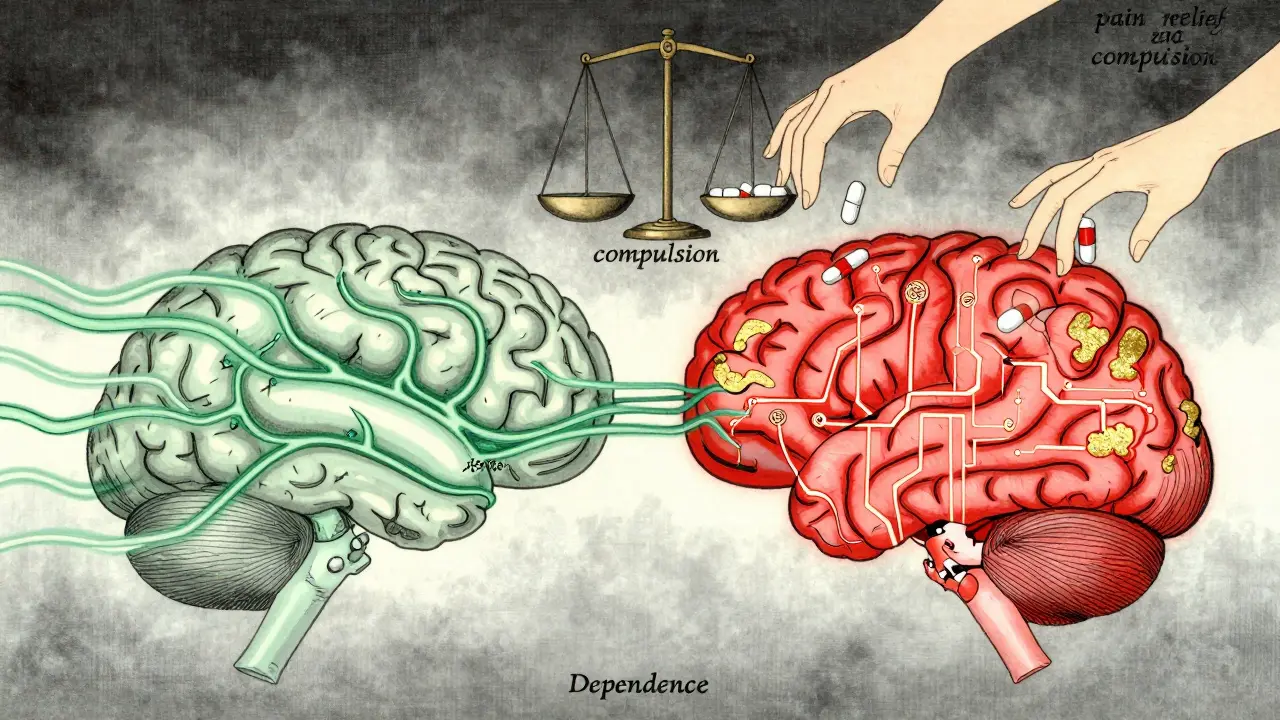
Addiction-now called Opioid Use Disorder (OUD) in clinical terms-is not about withdrawal. It’s about behavior. The American Psychiatric Association’s DSM-5 defines it as a chronic brain disorder where compulsive drug use continues despite serious harm. This isn’t about willpower. It’s about brain changes.Unlike physical dependence, which affects autonomic systems, OUD rewires the reward circuit. The mesolimbic dopamine pathway, the nucleus accumbens, the prefrontal cortex-all these areas get altered. Dopamine responses become distorted. The brain starts valuing the drug more than food, family, or safety. Neuroimaging shows a 20-30% drop in prefrontal cortex activity during impulse control tasks in people with OUD. That’s why someone might steal money, lie to doctors, or drive hours to get pills-even after losing their job or relationship.
The DSM-5 lists 11 criteria for OUD. You need at least two in a 12-month period. The most telling ones:
- Craving (present in 83% of severe cases)
- Loss of control over use
- Continuing use despite physical or psychological harm
- Failing to meet work, school, or family obligations
- Spending excessive time getting, using, or recovering from the drug
Here’s the key: You can be physically dependent without any of these. And you can have OUD without obvious withdrawal symptoms. Some people with OUD don’t even experience strong withdrawal because they keep using to avoid it. That’s the trap.
Why the Confusion Exists-and Why It’s Harmful
A 2020 study in the Journal of Pain Research found that 68% of chronic pain patients on opioids believed withdrawal meant they were addicted. That’s not just misinformation. It’s a public health crisis. Many patients stop their medication out of fear. Others are dismissed by doctors who assume dependence equals addiction.One patient on Reddit wrote: “I tapered off 60 MME/day oxycodone over 8 weeks. Had withdrawal for 10 days. Never wanted to use recreationally. Never lied to get more. I just needed the pills for my back.” That’s physical dependence. Clean, clear, medical.
Another patient shared: “After my surgery, I kept refilling prescriptions I didn’t need. I stole from my mom. I drove two hours to get more pills. I lost my job. I didn’t care.” That’s OUD. The behavior is the diagnosis.
Conflating the two has real consequences. In 2021, the American Medical Association passed a resolution urging doctors to stop treating physical dependence like addiction. The CDC’s 2022 guidelines explicitly state: “Physical dependence is not a reason to discontinue opioid therapy when benefits outweigh risks.” Yet, many clinics still cut patients off cold turkey. That’s not treatment. It’s abandonment.

How Doctors Tell the Difference
There’s no single blood test. But there are tools. The Opioid Risk Tool (ORT) helps identify who’s at higher risk for developing OUD. About 24% of patients score as high-risk based on family history, mental health, or past substance use.For those developing physical dependence, the CDC recommends tapering slowly: 5-10% dose reduction every 2-4 weeks. For patients on over 100 MME/day, go slower-5% per month. Withdrawal symptoms are tracked using the Clinical Opiate Withdrawal Scale (COWS). A score above 12 means moderate withdrawal and needs medical support.
For OUD, diagnosis relies on the DSM-5 criteria, administered by trained clinicians. Studies show this method is 94% accurate. If someone meets 6 or more criteria, they have severe OUD. That’s when Medication-Assisted Treatment (MAT) becomes essential. Buprenorphine cuts mortality by 70-80%. Methadone reduces it by 50%. These aren’t substitutes. They’re medical treatments that stabilize the brain so therapy can work.
What Treatment Looks Like for Each
If you’re physically dependent, the goal is safe discontinuation. That means a slow taper, maybe with lofexidine (a non-opioid medication approved in 2023 to ease withdrawal symptoms), and support for nausea, sleep, or anxiety. No therapy needed unless you have underlying depression or trauma.If you have OUD, the goal is recovery. That means MAT plus counseling. Medications like buprenorphine block cravings and normalize brain function. Behavioral therapy addresses the root causes: trauma, isolation, untreated mental illness. You can’t taper your way out of OUD. The brain has changed. You need to rewire it.
Insurance coverage reflects this divide. Nearly all commercial plans cover MAT under mental health parity laws. But only 67% have clear protocols for managing physical dependence during legitimate pain care. That’s a gap.
The Bigger Picture: Misdiagnosis Costs Lives
The opioid crisis didn’t start with illegal drugs. It started with doctors misunderstanding dependence. After the 2016 CDC guidelines, prescriptions dropped by 44%. But that didn’t reduce overdoses. It pushed people to heroin and fentanyl. Over 80,000 opioid-related deaths happened in 2021 alone.Why? Because patients who were dependent but not addicted were cut off. They had pain. They had no access to care. They turned to the streets.
Now, new tools are emerging. A 2023 study in the Journal of Neuroscience used fMRI to measure prefrontal cortex activity during craving tasks. It could tell physical dependence from OUD with 89% accuracy. That’s huge. Within 3-5 years, this could become standard practice.
Right now, misdiagnosis rates are still around 35%. That means 1 in 3 people are being treated wrong. Either they’re being denied pain relief, or they’re being told they’re addicted when they’re not.
What You Need to Know
- Physical dependence = your body adapting. Withdrawal happens. It’s normal. Doesn’t mean you’re addicted.- Addiction (OUD) = compulsive use despite harm. Craving, lying, stealing, neglecting life. That’s the diagnosis.
- Tolerance isn’t addiction. It’s expected.
- Stopping opioids suddenly because of withdrawal? That’s not treatment. That’s a mistake.
- If you’re on long-term opioids and feel scared, talk to your doctor. Ask: “Am I dependent? Or am I addicted?”
- If you or someone you know is using opioids compulsively, help is available. MAT saves lives. It’s not giving up. It’s getting well.
Can you be physically dependent on opioids without being addicted?
Yes. Nearly everyone who takes opioids daily for more than a week develops physical dependence. This is a normal biological response. Addiction requires compulsive behavior, loss of control, and continued use despite harm. You can have dependence without addiction.
Does withdrawal mean I’m addicted?
No. Withdrawal symptoms like nausea, sweating, and anxiety are signs your body has adapted to the drug, not that you’re addicted. Many people experience withdrawal after taking opioids as prescribed for pain and never develop addictive behaviors.
How do I know if I have Opioid Use Disorder?
OUD is diagnosed when you have at least two of 11 specific behaviors over 12 months, including cravings, inability to cut down, neglecting responsibilities, and continuing use despite harm. If you’re taking opioids as directed and still functioning in life, you likely don’t have OUD.
Is tapering off opioids safe if I’m dependent?
Yes, when done slowly and under medical supervision. The CDC recommends reducing doses by 5-10% every 2-4 weeks. Faster tapers can trigger severe withdrawal and increase the risk of relapse or overdose. Never stop cold turkey.
Can someone with OUD ever recover without medication?
Some people do, but it’s rare and risky. Medication-Assisted Treatment (MAT) with buprenorphine or methadone reduces overdose deaths by 50-80%. Recovery without medication often involves high relapse rates. MAT isn’t replacing one drug with another-it’s stabilizing brain function so therapy and recovery can take hold.
Glendon Cone
December 31, 2025 AT 03:25Man, this is one of those posts that actually makes you stop and think. I’ve seen so many people panic because they get sick when they miss a dose, like it’s some moral failing. But nah, it’s just biology. My uncle was on opioids for spinal stenosis for 5 years, never chased highs, never lied, just needed to walk without crying. They tried to cut him off cold turkey-ended up in the ER with seizures. 😔
Kelly Gerrard
January 1, 2026 AT 22:37Physical dependence is not addiction. This is not a suggestion. It is a medical fact. If you confuse the two you are endangering lives. Period. Stop conflating physiology with pathology. Your ignorance is killing people. The AMA said so. The CDC said so. Why are you still arguing this?
Henry Ward
January 2, 2026 AT 19:55Oh wow so now we’re giving out gold stars for people who don’t steal from their moms? Congrats you took your pills on time. Meanwhile real addicts are out here living in alleys and you’re acting like you’ve solved world hunger. You’re not a hero. You’re just not a criminal. Big whoop.
Kunal Karakoti
January 4, 2026 AT 12:51It is interesting how the body adapts to chemical stimuli. The mind, however, is not so easily understood. Dependence is a physical phenomenon. Addiction is a metaphysical one. The brain changes, yes-but so does the soul's relationship to suffering. Are we treating the neuron or the narrative?
Aayush Khandelwal
January 5, 2026 AT 13:57Let’s not get lost in the pharmacological poetry here. Dependence = autonomic recalibration. OUD = dopaminergic hijacking. The neurocircuitry is clear. What’s messy is the stigma. And the insurance companies. And the docs who still think ‘addiction’ means ‘bad person.’ We need more MAT access, not more moralizing. 🤝
Sandeep Mishra
January 6, 2026 AT 02:26Hey everyone-just want to say this is one of the clearest breakdowns I’ve seen on this topic. If you’re reading this and scared you’re addicted because you feel sick when you skip a pill-take a breath. You’re not broken. You’re just human. And if you’re a clinician reading this-please, don’t cut people off. We’ve done enough damage already. 💙
Colin L
January 7, 2026 AT 23:03Let’s be honest here-this entire discussion is a distraction. The real issue isn’t whether dependence equals addiction-it’s that we’ve allowed Big Pharma to weaponize pain management for profit. We’ve created a system where people are either overmedicated or abandoned, with no middle ground. The science is fine. The system is broken. And until we fix that, all these definitions are just rearranging deck chairs on the Titanic.
Hayley Ash
January 8, 2026 AT 20:35So what you’re saying is if I steal my neighbor’s pain meds and lie to 3 doctors but don’t throw up when I miss a dose I’m addicted but if I just feel shaky and nauseous I’m just ‘physically dependent’? Wow. That’s some next level semantics. So addiction is just a bad behavior checklist now? Cool. I’ll just print it out and use it as a bingo card at my next AA meeting. 😏
kelly tracy
January 9, 2026 AT 14:23Everyone’s so quick to defend the ‘good addicts’ while ignoring the fact that 90% of people on long-term opioids are just lazy and don’t want to deal with real pain. You think your back pain is special? Everyone’s in pain. You just don’t want to move. This isn’t medicine. It’s an excuse to sit on the couch and scroll TikTok.
srishti Jain
January 10, 2026 AT 07:25Dependence = bad. Addiction = worse. Either way you’re a junkie. Just admit it.
Nadia Spira
January 11, 2026 AT 19:00It’s fascinating how we’ve anthropomorphized neurochemistry. We say the brain ‘rewires’ like it’s a conscious architect. But the brain doesn’t want anything. It’s a biological machine. To call OUD a ‘brain disorder’ is just rebranding moral failure with neurobabble. You’re not sick-you’re weak. And no pill will fix that.
henry mateo
January 12, 2026 AT 16:03i just wanted to say thank you for writing this. my dad was on oxycodone for 12 years after his accident. he never got high, never lied, just needed to stand up. when they cut him off he tried to kill himself. i wish more people understood this. sorry for the typos. typing with tears.
Joseph Corry
January 13, 2026 AT 13:43Let’s not pretend this is a neutral scientific discourse. You’re romanticizing dependence as if it’s some noble physiological state. But dependence is a gateway. It normalizes use. It erodes boundaries. And every ‘good patient’ you defend is one more person who could slide into OUD when life gets hard. This isn’t harm reduction. It’s denial dressed in lab coats.