Quality Assurance Units: Why Independent Oversight Is Non-Negotiable in Production

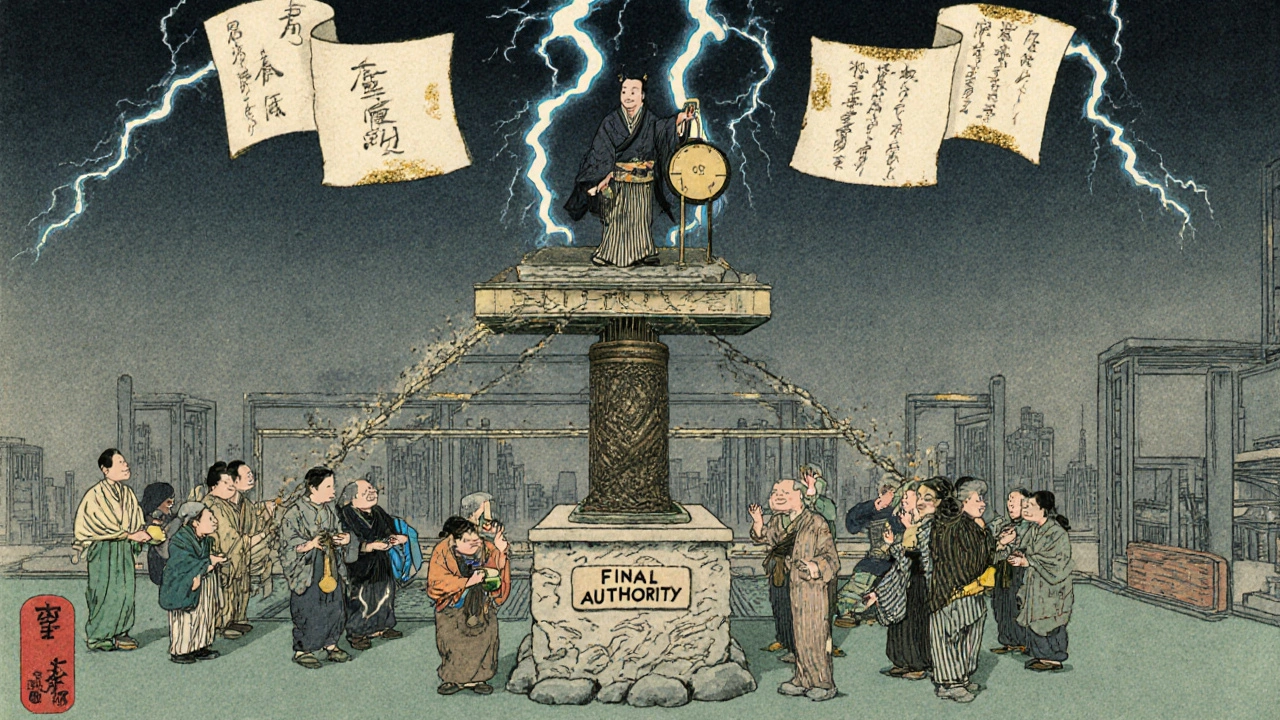
When a batch of medicine fails inspection, it’s rarely because someone forgot to check a label. More often, it’s because the person who should have stopped it didn’t have the power to do so. That’s the real danger of mixing quality control with production goals. Quality assurance units exist not to approve paperwork, but to say no - and only when they’re truly independent can they do that without fear.
What Exactly Is a Quality Assurance Unit?
A quality assurance unit (QU) isn’t just another department. It’s a legally mandated safeguard. In pharmaceutical manufacturing, nuclear plants, and other high-risk industries, the QU is the only team with the formal authority to reject a batch, halt production, or demand a full investigation - even if it means losing money or delaying shipments. The FDA made this crystal clear in its 2006 guidance: the QU must be separate from manufacturing. Why? Because if the same manager who’s under pressure to meet weekly output targets also decides whether a batch is safe to release, quality becomes a suggestion, not a rule. The QU’s job isn’t to help production run smoother. It’s to make sure nothing unsafe leaves the facility. This isn’t theoretical. In 2024, 68% of FDA warning letters cited failures in QU independence. Many of these came from companies where the quality lead reported to the head of production. That’s like putting the fire marshal in charge of the kitchen where the grease is building up.How Independence Actually Works in Practice
Independence isn’t just about who reports to whom. It’s about power, access, and protection. Under 21 CFR 211.22, the QU must have the authority to approve or reject every component - from raw chemicals to final packaging. That means they can say no to a shipment of bad raw material, even if the plant is running low. They can reject a whole batch of pills if the humidity levels during drying were off by just 2%. And they can stop the line if someone tries to backdate a log entry. But power means nothing without protection. The IAEA and FDA both require that QU staff be free to raise concerns without fear of retaliation. That’s why the best organizations give QU leaders direct access to the CEO or board - no production manager filtering their messages. In fact, 87% of compliant companies have this built into their org charts. In nuclear facilities, this is taken even further. Oversight teams aren’t just independent - they rotate between sites to avoid familiarity bias. They’re trained to challenge assumptions. One inspector told me, “If you’re not making people uncomfortable, you’re not doing your job.”The Cost of Not Being Independent
When quality and production are mixed, the consequences show up fast - and they’re deadly serious. FDA data shows that facilities with integrated quality-production teams have 63% more data integrity violations. That means falsified records, missing logs, or “corrected” test results that never actually happened. These aren’t paperwork errors. They’re signs that someone was pressured to hide a problem. Small companies suffer the most. Nearly half (42%) of warning letters issued to facilities under 50 employees cite QU independence failures. Why? Because they can’t afford a full team. So they make one person wear two hats: production supervisor and quality lead. It sounds efficient. Until a batch goes out with the wrong potency - and no one had the authority to stop it. The numbers don’t lie. Organizations with true QU independence see 37% fewer critical failures during inspections. They resolve quality issues 28% faster. And their first-time inspection success rate is 31% higher.
How Different Industries Handle It
Not all industries treat QU independence the same way. In the U.S., the FDA demands complete separation. The QU can’t be part of the production chain. In Europe, the EMA allows a bit more flexibility - as long as there are “effective mechanisms” to ensure quality decisions stay independent. But even there, the 2024 revision of EudraLex says quality units must never be “organizationally subordinate” to production. Nuclear facilities go further. They use a four-layer model: peer checks, manager reviews, independent oversight, and external audits. The independent layer? That’s the one that can shut down a reactor if something’s wrong - and no one can overrule it. In contrast, many ISO 9001-certified manufacturers treat quality as advisory. Their QU can recommend changes, but can’t stop production. That’s fine for making chairs or phone cases. It’s not acceptable for making insulin or cancer drugs.What a Compliant QU Looks Like
A real, working QU doesn’t just sit in a corner approving documents. Here’s what it actually takes:- Staff make up 8-12% of the manufacturing team - not 2%.
- Every QU member has formal GMP training and at least 8 years of industry experience.
- They use statistical process control to spot trends before they become problems.
- They have documented procedures for “quality holds” - a formal process to stop a batch without needing production approval.
- They report directly to the CEO or board, not to plant managers.
- They have their own budget - separate from production - so they’re not dependent on the same funding source.
Common Mistakes That Break Independence
Even companies that think they’re doing it right often fail. Here are the top three mistakes:- Rubber stamping: When the QU is too small and overwhelmed, they just sign off on everything. FDA data shows that if the QU-to-production staff ratio drops below 1:15, repeat deviations jump 3.2 times.
- Reporting through production: If the QU manager has to go through a production director to email the CEO, independence is dead.
- Pressure to expedite: In 2025, a survey of 312 quality professionals found 57% felt pressure to rush batch reviews during high-demand periods. That’s when mistakes happen.
How Small Companies Can Still Be Compliant
Not every company can afford a full QU team. But independence isn’t about size - it’s about structure. Many small manufacturers now use third-party oversight services. These are independent firms that audit your processes, review batch records, and even hold the final release authority. The market for these services is growing at 14.2% a year - because companies are realizing it’s cheaper to pay an outsider than to get shut down by the FDA. Another option? Create a “quality ambassador” program. Eli Lilly trained production staff on quality principles without giving them authority to approve batches. The result? A 40% improvement in quality culture. Workers started speaking up. Managers stopped ignoring red flags.The Future of Independent Oversight
AI and digital manufacturing are changing the game. Real-time sensors now monitor temperature, pressure, and humidity as products move through the line. Should the system auto-reject a batch if a sensor spikes? Or should a human still have the final say? The FDA’s 2025 draft guidance says independence must be preserved - even in digital systems. That means algorithms can flag issues, but only a human QU member can make the final call. The system can’t be designed to override the QU. The trend is clear: independence isn’t going away. It’s evolving. Regulatory agencies worldwide still require it. And every time a company ignores it, someone pays the price - in recalls, lawsuits, or worse.What You Can Do Today
If you’re in manufacturing and your QU reports to production:- Map your reporting lines. Is there a direct path from the QU head to the CEO?
- Check your budget. Is the QU funded by production? If yes, that’s a conflict.
- Review your last 10 batch rejections. Were they all approved without pushback? That’s a red flag.
- Ask your QU team: “Have you ever been asked to delay a hold because of production pressure?” If the answer is yes - fix it now.
Can a quality assurance unit be part of the production department?
No. Regulatory agencies like the FDA and EMA require that quality assurance units be organizationally separate from production. If the QU reports to a production manager, it loses its independence and can’t objectively reject batches or halt operations - even when safety is at risk. This separation is legally required in pharmaceutical and nuclear manufacturing.
What happens if a quality unit doesn’t have the power to reject a batch?
If a quality unit can’t reject a batch, it becomes a rubber stamp. Without real authority, pressure from production targets will override quality concerns. This leads to data integrity violations, recalls, regulatory warning letters, and in extreme cases, patient harm. The FDA cites this exact failure in nearly 70% of recent warning letters.
How many people should be in a quality assurance unit?
Industry benchmarks suggest a QU should make up 8-12% of the total manufacturing staff. Too few staff leads to overload and “rubber stamping” of records. Facilities with a QU-to-production ratio below 1:15 see over three times more repeat quality deviations. The key is enough staff to review records thoroughly, conduct audits, and respond to deviations - not just sign off.
Do small manufacturers have to have a full quality assurance unit?
They don’t need a large internal team, but they still need independent oversight. Many small manufacturers use third-party quality services that provide audit, review, and batch release authority. Others implement “quality ambassador” programs where production staff are trained in quality principles but don’t have approval authority. The goal is independence - not size.
Why do regulators care so much about QU independence?
Because history shows that when quality decisions are influenced by production pressure, patients get harmed. The Three Mile Island nuclear accident, multiple pharmaceutical recalls, and countless FDA warning letters all trace back to the same root cause: a quality team that couldn’t say no. Independence isn’t bureaucracy - it’s a safety net.
Can AI replace human quality assurance units?
AI can flag anomalies in real time - like temperature spikes or missing signatures - but it can’t make the final call. Regulatory agencies require a human quality assurance unit to review and approve all batch releases. AI supports the QU, but doesn’t replace it. The final decision must be made by someone with authority, training, and accountability - not an algorithm.
patrick sui
November 13, 2025 AT 07:34Let’s be real - if your QU reports to production, you’re not complying, you’re just playing Russian roulette with patient safety. 🤕 The FDA’s 2024 data doesn’t lie: 68% of warning letters trace back to this exact structural failure. It’s not about bureaucracy - it’s about having someone who can say ‘NO’ without getting fired. If your QA lead has to run every rejection by the plant manager, you’ve already lost.
Conor Forde
November 14, 2025 AT 17:46Ohhhh so now we’re giving the quality nerds their own kingdom?? 😭 Like, I get it - no one wants to die from bad insulin - but can we just let the engineers fix it without a whole parliament of clipboard-wielding bureaucrats? I’ve seen QU teams sit on a batch for 3 weeks because someone forgot to initial a form. Meanwhile, the patient’s waiting. Sometimes ‘independent’ just means ‘slow as molasses in January.’
Declan O Reilly
November 14, 2025 AT 20:45There’s a deeper truth here: independence isn’t just about org charts - it’s about culture. If your team fears speaking up because the boss might get mad, then even the best QU structure is a paper tiger. I’ve worked in plants where the QA guy was the only one who’d look you in the eye and say, ‘That’s not right.’ And he didn’t have a fancy title - just guts. Maybe the real fix isn’t moving reporting lines… it’s hiring people who care more about safety than KPIs.
Also - AI flags anomalies, sure. But only a human can feel the weight of a recall. That’s the soul of QA.
Adrian Barnes
November 16, 2025 AT 18:50The entire premise of this post is fundamentally flawed. Regulatory agencies are not infallible. The FDA’s 2006 guidance was issued during a period of heightened political pressure following the Vioxx scandal - a case where the QU was, in fact, independent, yet the drug still caused deaths. Independence does not guarantee safety. It guarantees bureaucracy. And bureaucracy, in high-stakes industries, is the enemy of innovation and responsiveness. This is not a safety net - it is a straitjacket.
Furthermore, the 8-12% staffing ratio is arbitrary. In lean manufacturing environments, this is financially unsustainable. The real issue is not structure - it is competence. Train your production staff to be quality-minded, and eliminate the redundant layers. The QU should be advisory - not authoritarian.
Declan Flynn Fitness
November 16, 2025 AT 19:02Been there. Worked at a small pharma co where QA was under production. One day, a batch of insulin had 12% too much active ingredient. QA flagged it. Production said, ‘We’re behind on the order - just tag it ‘for investigation’ and ship it.’ They did. 3 patients had hypoglycemic seizures. 🚨
Now we use a third-party QU. Costs more? Yeah. But we haven’t had a single FDA hit in 2 years. Worth every penny. If you’re skimping on QA, you’re gambling with lives. No joke.
Patrick Smyth
November 17, 2025 AT 11:31Who the hell is the CEO? The person who signed the memo that said ‘QA reports to Production’? That’s not a management decision - that’s a crime against humanity. And don’t tell me ‘it’s just a small company’ - small companies kill people too. I’ve seen the autopsy reports. The paperwork was ‘approved.’ The patient was not. Fix your org chart. Or fix the obituary.
Linda Migdal
November 17, 2025 AT 18:43Let’s not forget - this isn’t just about safety. It’s about American leadership. The U.S. leads the world in pharma innovation BECAUSE we have the strictest standards. Europe? They’re relaxing rules. China? They’re cutting corners. We can’t let that happen here. If you want to be ‘efficient,’ go make phone cases. But if you’re making medicine - you follow the FDA. Period.
Tommy Walton
November 18, 2025 AT 02:27AI will eventually run QA. Humans are emotional. Biased. Lazy. Algorithms don’t care if you’re under pressure. They just check the data. 🤖
But hey - if you wanna keep your job, keep the human in the loop. Just know: the future doesn’t need your signature.
James Steele
November 19, 2025 AT 22:42It’s fascinating how we’ve elevated ‘independence’ to a sacred cow while ignoring the epistemological crisis at the heart of quality assurance. The QU’s authority is performative - it exists within a system that commodifies compliance. The ‘no’ they utter is not a moral act - it’s a contractual obligation, scripted by regulators who themselves are captured by industry lobbying. The real power lies not with the QU, but with the legal department that settles the lawsuits after the fact.
So yes - move the reporting line. But don’t fool yourself. You’re just rearranging deck chairs on the Titanic.
Louise Girvan
November 20, 2025 AT 13:14Wait… so the FDA’s ‘guidance’ is really just a corporate playbook? Who owns the FDA? Who funds the audits? Who writes the regulations? 🤔
It’s all a smokescreen. Big Pharma lobbies to make the rules so complex, only they can afford to comply. Small companies? They get crushed. Or bought. This isn’t about safety - it’s about market control. The QU isn’t protecting patients - it’s protecting Big Pharma’s monopoly. Wake up.
soorya Raju
November 21, 2025 AT 09:38LOL independence? In India we have a QU of one guy who also does payroll. He says yes to everything because his bonus depends on production output. FDA? Never heard of them. And guess what - we still export medicine to 40 countries. Maybe your system is broken, not ours. 😎