Sleep Apnea and Respiratory Failure: How Oxygen Therapy and CPAP Work Together
When your breathing stops repeatedly during sleep, your body doesn’t just wake you up-it stresses your heart, floods your blood with carbon dioxide, and drops oxygen levels to dangerous spots. This isn’t just snoring. This is obstructive sleep apnea (OSA), and if left untreated, it can lead to respiratory failure. For millions of people, the solution isn’t surgery or pills-it’s a simple machine that blows air into your airway while you sleep. That machine is CPAP. But oxygen therapy? That’s not always the answer, even though it sounds logical.
Why CPAP Is the Gold Standard, Not Just Oxygen
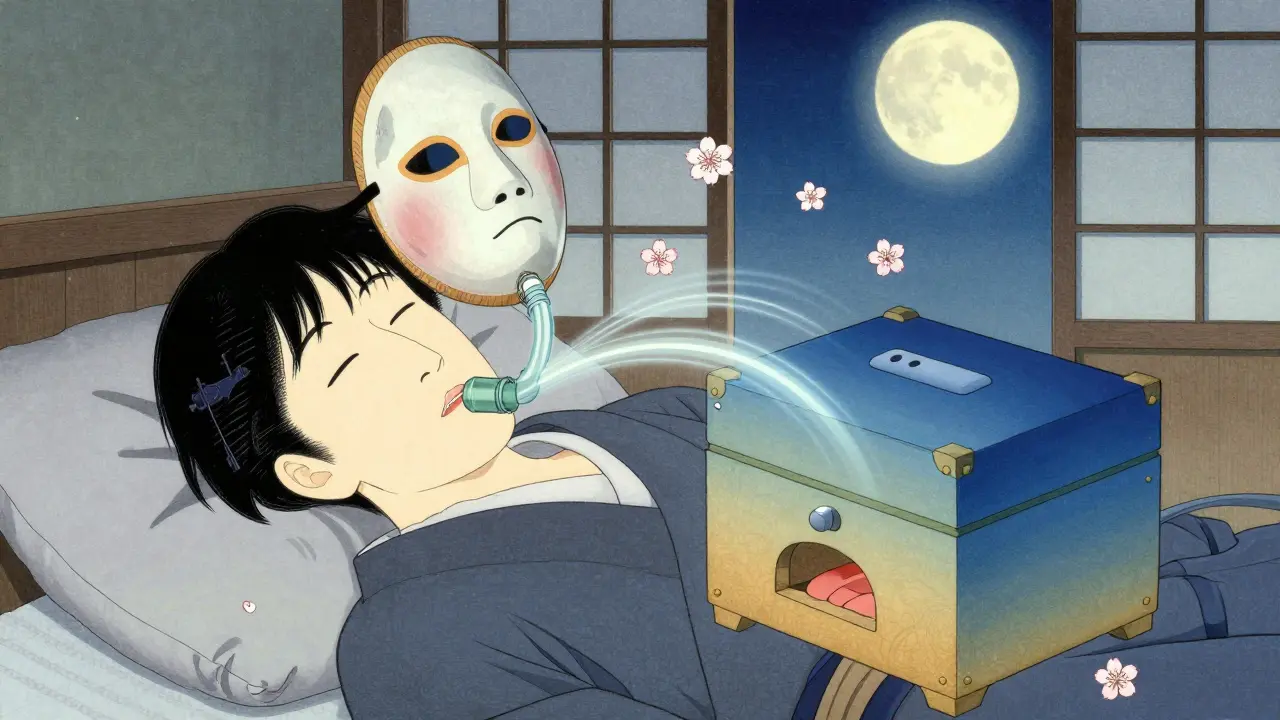
Many people assume that if sleep apnea causes low oxygen, then giving more oxygen should fix it. It doesn’t. Oxygen therapy treats the symptom-low blood oxygen-but it ignores the root cause: your airway collapsing. Think of it like putting a bandage on a leaking pipe instead of fixing the crack. CPAP, on the other hand, acts like a pneumatic splint. It keeps your throat open with steady air pressure, stopping the collapse before it happens. Studies show that when patients use CPAP correctly, their apnea-hypopnea index (AHI)-the number of breathing pauses per hour-drops from 30-40 to under 5 in 90% of cases. That’s not improvement. That’s resolution. Oxygen masks might raise your oxygen levels a bit, but they don’t reduce those pauses. You still wake up dozens of times a night. You still feel exhausted. You still risk high blood pressure, heart attacks, and stroke.How CPAP Actually Works
A CPAP machine takes room air, pressurizes it, and delivers it through a hose to a mask you wear while sleeping. The pressure is usually between 4 and 20 centimeters of water (cm H₂O)-enough to hold your tongue and soft palate from falling back and blocking your throat. Most people use a nasal mask (73% do), but full-face masks or nasal pillows are options if you breathe through your mouth or have nasal congestion. There are different types of machines:- Fixed CPAP: Delivers one steady pressure all night.
- Auto-CPAP (APAP): Adjusts pressure automatically based on your breathing patterns. Good for people whose needs change from night to night.
- BiPAP: Gives higher pressure when you inhale and lower pressure when you exhale. Helps if you struggle to breathe out against the constant pressure or need higher settings above 15 cm H₂O.
Why People Stop Using CPAP (And How to Fix It)
The biggest problem with CPAP isn’t the machine-it’s the user. About half of people quit within the first year. Why? Mask discomfort, dry mouth, claustrophobia, and noise. But most of these problems are fixable. - Mask leaks? Try a different style. Nasal pillows are less intrusive. Chin straps help if you open your mouth.When Oxygen Therapy Actually Makes Sense
Oxygen therapy isn’t useless-it just doesn’t treat OSA. It’s used when there’s another condition: chronic lung disease like COPD, pulmonary fibrosis, or severe heart failure. In those cases, the lungs can’t move oxygen into the blood well enough, even if the airway is open. That’s when supplemental oxygen helps. But here’s the catch: if you have both OSA and COPD (a condition called overlap syndrome), you might need both CPAP and oxygen. CPAP keeps your airway open. Oxygen makes sure your blood gets enough. Doctors test for this with overnight sleep studies that measure both breathing events and blood oxygen levels.
What About Central Sleep Apnea?
Not all sleep apnea is caused by a blocked airway. In central sleep apnea (CSA), your brain just doesn’t tell your body to breathe. This often happens in people with heart failure or after a stroke. CPAP doesn’t work well here. Instead, doctors use:- ASV (Adaptive Servo-Ventilation): Adjusts pressure in real time to support breathing rhythm. Reduces central apneas by 68%.
- BiPAP with backup rate: Gives you a breath if you don’t breathe on your own for a few seconds.
CPAP and Your Heart
Sleep apnea doesn’t just make you tired. It raises your blood pressure. It increases inflammation. It strains your heart. CPAP lowers systolic blood pressure by 2.5 to 5 mmHg on average-similar to what you’d get from cutting salt or losing 10 pounds. In heart failure patients with OSA, CPAP improves left ventricular ejection fraction by 4-6%. That’s the heart’s ability to pump blood. Better pumping means fewer hospital visits. But here’s the twist: the SAVE trial found that CPAP didn’t reduce heart attacks or strokes in people with OSA who already had heart disease-and weren’t sleepy. That means CPAP isn’t a magic bullet for everyone. If you’re not tired during the day, your doctor might question whether the benefits outweigh the hassle.What’s Next? New Tech Is Coming
CPAP has been the standard since 1981. But it’s not the only option anymore. In 2023, the FDA approved the first implantable device for OSA: the hypoglossal nerve stimulator (Inspire). It’s like a pacemaker for your tongue. It senses when you’re breathing and gently stimulates the nerve to keep your tongue forward. In trials, 79% of users stuck with it after a year-compared to 46% for CPAP. It’s not for everyone. You need to be a certain size, have moderate-to-severe OSA, and not be obese. But it’s a real alternative. New CPAP machines now come with remote monitoring. Your machine sends data to your doctor’s office. If your pressure needs change, or you’re not using it enough, they’ll call you. ResMed’s AirView platform cut follow-up visits by 27%. No more waiting weeks for a clinic appointment.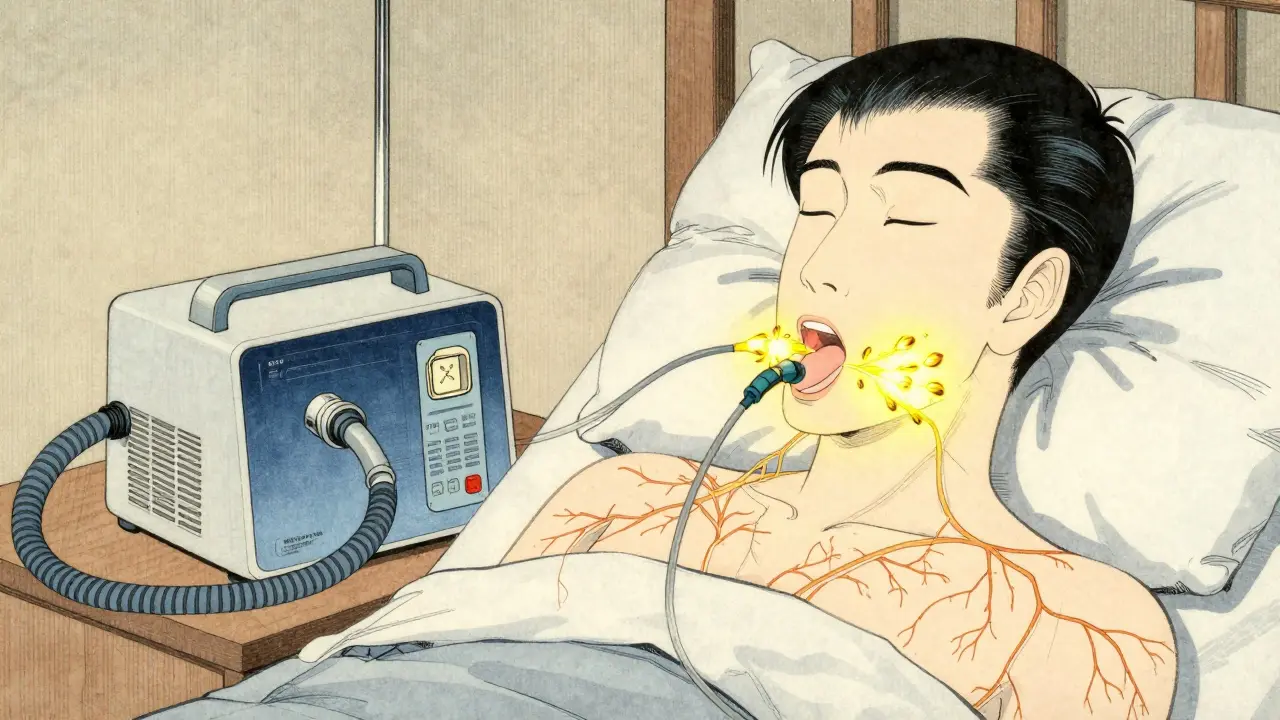
How to Know If You’re Getting Real Results
Adherence isn’t just about hours per night. The American Thoracic Society says you need more than 4 hours on 70% of nights. But that’s just the start. Better goals now include:- AHI under 5
- Mask leak under 24 liters per minute
- Daytime alertness improvement (most people feel better in 1-2 weeks)
- Lower blood pressure readings
Insurance, Cost, and Getting Started
In the U.S., Medicare pays about $209.74 per month for CPAP equipment. Most private insurers cover it too-but only if you prove you’re using it. Around 45% of insurers now require you to use CPAP at least 4 hours a night, 70% of the time, to keep getting coverage. The machines themselves cost between $500 and $1,200, but insurance usually handles most of it. What you pay out of pocket depends on your plan. Don’t skip the sleep study. Without a diagnosis, you won’t get insurance approval.What to Do If CPAP Isn’t Working
If you’ve tried everything and still can’t use CPAP:- Ask about oral appliances (mandibular advancement devices). They’re less effective for severe OSA but better tolerated. 70% stick with them after a year.
- Check for nasal obstruction. A deviated septum or chronic sinusitis can make CPAP feel impossible. ENT evaluation might help.
- Consider surgery only as a last resort. UPPP or tongue reduction have low success rates and high complication risks.
- Explore Inspire therapy if you qualify. It’s not cheap, but it’s FDA-approved and covered by many insurers now.
Final Thought: This Isn’t a Quick Fix-It’s Lifelong Care
Sleep apnea is a chronic condition. Like diabetes or high blood pressure, it needs daily management. CPAP isn’t a cure, but it’s the most effective tool we have. The machines are quieter, smaller, and smarter than ever. The support is better. The data is real. If you’re struggling, you’re not alone. 68% of users report better alertness within two weeks. But 42% quit because of discomfort. Don’t be one of them. Reach out. Try a different mask. Ask for humidification. Get help. Your heart, your brain, and your future self will thank you.Can oxygen therapy treat sleep apnea?
No. Oxygen therapy raises blood oxygen levels but doesn’t stop the airway from collapsing during sleep. It treats the symptom, not the cause. CPAP is needed to keep the airway open. Oxygen may be added in cases of overlap syndrome (OSA + COPD), but alone, it won’t fix sleep apnea.
How long does it take to feel better after starting CPAP?
Most people notice improved alertness and reduced daytime fatigue within 1 to 2 weeks. Some feel better after just a few nights. But full benefits-like lower blood pressure and better mood-can take 3 to 6 months of consistent use. Don’t give up if you don’t feel a difference right away.
Is CPAP the only treatment for obstructive sleep apnea?
No. For mild cases, weight loss, positional therapy (sleeping on your side), or oral appliances can help. For moderate to severe cases, CPAP is the gold standard. New options like hypoglossal nerve stimulation (Inspire) are now available for patients who can’t tolerate CPAP. Surgery is rarely recommended due to lower success rates and higher risks.
Why do some people fail CPAP even when they try hard?
Common reasons include mask discomfort, dry mouth, nasal congestion, or incorrect pressure settings. Sometimes, the diagnosis is wrong-up to 28% of treatment failures are due to undiagnosed central sleep apnea. Other times, underlying issues like allergies or a deviated septum make breathing through the nose hard. A follow-up sleep study or ENT evaluation can help identify these hidden problems.
Does insurance cover CPAP machines?
Yes, most insurance plans, including Medicare and Medicaid, cover CPAP machines after a diagnosis from a sleep study. However, many insurers require proof of use-typically 4 hours per night on at least 70% of nights over 30 days. If you don’t meet these thresholds, coverage may stop. Always check your plan’s specific requirements.
Can I travel with my CPAP machine?
Yes. Most modern CPAP machines are compact and designed for travel. Many weigh under 2 pounds and can run on battery power or 12-volt car adapters. Airlines allow them as medical devices, so you can bring them on board. Always carry a doctor’s note and keep your machine in your carry-on. Altitude changes can affect pressure, so auto-adjusting models (APAP) are best for mountain trips.
What happens if I stop using CPAP?
Your sleep apnea symptoms will return within days. Snoring, breathing pauses, and low oxygen levels come back. Daytime sleepiness, poor concentration, and high blood pressure return too. Long-term, stopping CPAP increases your risk of heart attack, stroke, and irregular heart rhythms. It’s not safe to quit without talking to your doctor.
Akshaya Gandra _ Student - EastCaryMS
January 4, 2026 AT 10:51en Max
January 4, 2026 AT 23:27Peyton Feuer
January 6, 2026 AT 19:40Doreen Pachificus
January 7, 2026 AT 04:32Cassie Tynan
January 8, 2026 AT 07:39Rory Corrigan
January 8, 2026 AT 16:11Connor Hale
January 8, 2026 AT 16:37Oluwapelumi Yakubu
January 10, 2026 AT 13:32Joseph Snow
January 12, 2026 AT 12:32melissa cucic
January 13, 2026 AT 06:30Shanna Sung
January 15, 2026 AT 04:04Allen Ye
January 16, 2026 AT 17:54John Ross
January 17, 2026 AT 18:26