SNRI Medications: Extended Treatment Options for Mental Health

When antidepressants don’t work the way they should, doctors often turn to SNRI medications - not because they’re stronger, but because they work differently. Unlike SSRIs that only target serotonin, SNRIs affect two key brain chemicals: serotonin and norepinephrine. This dual action makes them especially useful for people struggling with depression along with fatigue, poor concentration, or chronic pain. If you’ve tried one or two SSRIs and still feel stuck, SNRIs might be the next step - not a magic fix, but a real alternative backed by years of clinical use.
How SNRIs Actually Work
SNRI stands for Serotonin and Norepinephrine Reuptake Inhibitor. That’s a mouthful, but here’s what it means in plain terms: your brain uses these two chemicals to help regulate mood, energy, focus, and even how you experience pain. After neurons send signals using serotonin and norepinephrine, they normally suck those chemicals back up to reuse them. SNRIs block that reabsorption, leaving more of both chemicals floating around in the spaces between brain cells. This helps messages get through more clearly.
Not all SNRIs work the same way. Venlafaxine (Effexor XR) and desvenlafaxine (Pristiq) start off acting mostly like SSRIs at low doses - meaning they focus on serotonin. But when the dose goes up past 150 mg/day, they kick in on norepinephrine too. Duloxetine (Cymbalta) and levomilnacipran (Fetzima), on the other hand, hit both neurotransmitters from the first pill. This matters because it affects how quickly you might feel changes - and what side effects you get.
Approved Uses Beyond Depression
The FDA hasn’t just approved SNRIs for depression. They’re also cleared for:
- Generalized anxiety disorder - duloxetine and venlafaxine are both used for this.
- Diabetic nerve pain - duloxetine is one of the few pills proven to reduce burning, tingling, or numbness in feet and hands.
- Fibromyalgia - studies show about 35-40% of people on duloxetine get at least 50% pain relief.
- Chronic musculoskeletal pain - including lower back pain and osteoarthritis.
- Pediatric anxiety - in 2022, the FDA approved Drizalma Sprinkle (a form of duloxetine in granules) for children aged 7-17 with anxiety disorders.
This broad range of uses isn’t an accident. Norepinephrine doesn’t just lift mood - it also plays a big role in how your body processes pain signals. That’s why SNRIs often help people who feel emotionally drained and physically worn out.
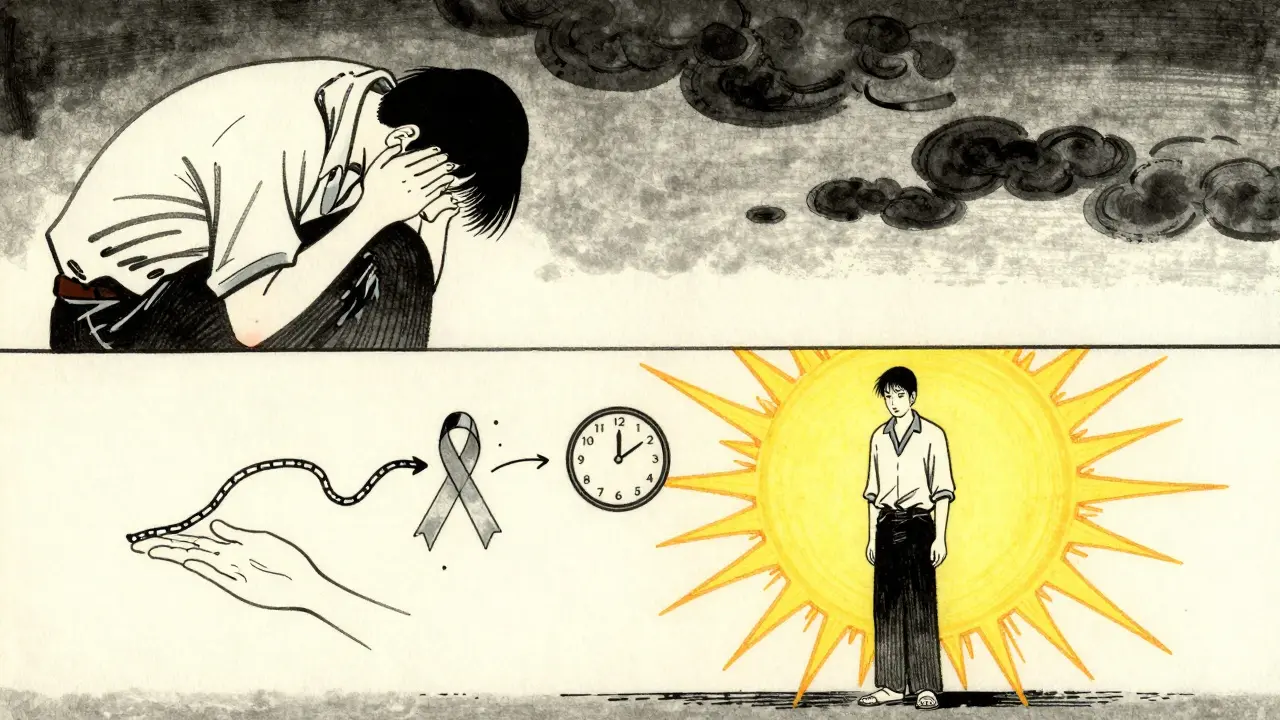
How Long Does It Take to Work?
Don’t expect results after a few days. Like most antidepressants, SNRIs take time. Most people start noticing small improvements in energy or sleep after 2-3 weeks. But real symptom relief - especially for pain or deep fatigue - often takes 6-12 weeks. A 2023 Cleveland Clinic review found that 40% of patients didn’t see major changes until after 8 weeks. If you stop too soon because you feel nothing, you might miss out on something that could truly help.
One big advantage? SNRIs don’t usually cause the same level of sedation or weight gain as older antidepressants like tricyclics. But they’re not side effect-free.
Common Side Effects and Risks
Every medication has trade-offs. For SNRIs, the most common issues include:
- Nausea - affects about 25% of people taking duloxetine. Usually fades after 1-2 weeks.
- Dizziness - happens in 15-20% of users, especially when standing up quickly.
- Insomnia - 10-15% report trouble sleeping, particularly with venlafaxine.
- Sexual side effects - decreased libido, delayed orgasm, or erectile dysfunction affect 20-30% of users.
- Blood pressure increase - up to 8% of patients develop higher readings, especially with venlafaxine. Doctors check BP every 2-4 weeks early on.
There’s also a risk of withdrawal symptoms if you stop suddenly. Called discontinuation syndrome, it can cause brain zaps (electric shock sensations), dizziness, nausea, and anxiety. About 20-30% of people who quit SNRIs abruptly experience this. But tapering slowly - over 4 to 6 weeks - cuts that risk down to under 10%.

SNRIs vs. SSRIs: What’s the Difference?
SSRIs like fluoxetine (Prozac) or sertraline (Zoloft) are still the first choice for depression. Why? They’re gentler. Fewer side effects, less risk of blood pressure spikes, and easier to stop. But they don’t always cut it for everyone.
Here’s how they compare:
| Feature | SSRIs | SNRIs |
|---|---|---|
| Primary target | Serotonin only | Serotonin + Norepinephrine |
| Typical response rate | 50-60% | 55-65% |
| Best for fatigue/pain? | Less effective | More effective |
| Common side effects | Nausea, sexual issues, weight gain | Nausea, dizziness, high BP, insomnia |
| Discontinuation risk | 15-25% | 20-30% |
| First-line use | Yes | Second-line |
SNRIs aren’t “better” than SSRIs - they’re just better for some people. If your depression comes with low energy, brain fog, or chronic pain, SNRIs often deliver more noticeable relief. But if you’re just dealing with sadness, irritability, or sleep issues without physical symptoms, an SSRI might be safer and simpler.
Real Patient Experiences
Online forums like Reddit and Drugs.com show mixed but revealing stories. One user wrote: “After three SSRIs failed, duloxetine cut my fibromyalgia pain in half. I still get nausea, but it’s worth it.” Another said: “I had brain zaps for weeks after stopping venlafaxine. Never again without a taper.”
A 2022 survey in the Journal of Affective Disorders found that 58% of SNRI users stayed on treatment for more than six months. That’s lower than SSRIs (65%), mostly because side effects pushed people to quit. But for those who stuck with it? 62% of respondents on Reddit said SNRIs gave them better energy and focus than anything else they’d tried.
How Doctors Start You on SNRIs
It’s not a “start high and see what happens” situation. Most providers begin low:
- Venlafaxine XR: Start at 37.5 mg daily, increase by 37.5 mg every 4-7 days.
- Duloxetine: Start at 30 mg daily, increase to 60 mg after 1-2 weeks.
- Desvenlafaxine: Start at 50 mg daily.
- Levomilnacipran: Start at 20 mg daily, increase to 40 mg after a week.
Doctors monitor blood pressure closely in the first month. They also watch for worsening anxiety or agitation in the first 2 weeks - especially in younger patients. The FDA requires a black box warning for all antidepressants: increased risk of suicidal thoughts under age 25. That doesn’t mean SNRIs cause it - but they can unmask it in vulnerable people.
Combining SNRIs With Therapy
Medication alone isn’t the full picture. A 2022 Mayo Clinic trial found that patients who took SNRIs and received cognitive behavioral therapy (CBT) had a 73% remission rate. Those on medication only? Just 48%. That gap tells you something important: SNRIs help your brain function better - but therapy helps you rebuild your life around it.
Many therapists now recommend combining talk therapy with SNRIs for depression with chronic pain. The medication eases the physical and emotional load; therapy helps you cope with limitations, adjust expectations, and find meaning again.
What’s Next for SNRIs?
Research is moving in two directions. First, personalized medicine. Some people metabolize SNRIs too fast or too slow because of genes like CYP2D6. Testing for these variants can now predict if a drug will work - or cause side effects - in about 60-70% of cases. It’s not routine yet, but it’s coming.
Second, combo therapies. A 2023 study in JAMA Network Open found that pairing duloxetine with a daily cognitive training app improved memory and focus in depressed patients by 35% more than the drug alone. Other trials are testing SNRIs with low-dose ketamine or psychedelic-assisted therapy - early results show remission rates jumping from 28% to 45%.
But here’s the reality: 30-40% of depression cases still don’t respond to any medication, including SNRIs. That’s why they’re not a cure-all. They’re a tool - one that works best when used with care, patience, and support.
When SNRIs Might Not Be Right
SNRIs aren’t for everyone. Avoid them if you:
- Have uncontrolled high blood pressure
- Take MAO inhibitors (a different class of antidepressant)
- Have a history of seizures
- Are pregnant or breastfeeding without clear medical guidance
- Have liver disease (especially for duloxetine)
Also, if you’ve had bad reactions to other antidepressants - especially withdrawal symptoms - SNRIs might not be the best next step. Talk to your doctor about alternatives like bupropion (which doesn’t affect serotonin) or newer options like vortioxetine.
Final Thoughts
SNRI medications aren’t the first answer for depression - but they’re one of the most useful second options. They shine when depression comes with physical symptoms: fatigue, pain, or difficulty concentrating. They’re not perfect. Side effects happen. Withdrawal can be rough. But for many, they’re the difference between barely getting by and feeling like yourself again.
If you’ve tried other antidepressants and still feel stuck, ask your doctor about SNRIs. Not as a last resort - but as a logical next step. And if you start one, give it time. Six weeks is the minimum. Twelve is better. And don’t stop without a plan. Taper slowly. Talk to your provider. Combine it with therapy if you can.
It’s not about finding the “best” drug. It’s about finding the right one - for you, right now.
Are SNRIs better than SSRIs for depression?
SNRIs aren’t necessarily better for pure depression. SSRIs remain first-line because they’re gentler and have fewer side effects. But SNRIs often work better when depression comes with fatigue, low energy, or chronic pain. Studies show SNRIs have slightly higher response rates - around 5-10 percentage points - in these cases. They’re not a replacement for SSRIs, but a different tool for different symptoms.
How long until SNRIs start working for pain?
For pain conditions like diabetic neuropathy or fibromyalgia, it can take 6-12 weeks to notice real improvement. Some people feel slight changes after 3-4 weeks, but full pain relief often takes longer than mood improvement. This is because nerve pain involves complex signaling pathways that take time to calm down. Don’t give up if you don’t feel better in the first month.
Can you stop SNRIs suddenly?
No. Stopping SNRIs abruptly can cause withdrawal symptoms like brain zaps, dizziness, nausea, anxiety, and insomnia. These are called discontinuation syndrome and affect 20-30% of people who quit cold turkey. To avoid this, taper slowly over 4-6 weeks under medical supervision. Never reduce your dose on your own.
Do SNRIs cause weight gain?
SNRIs are less likely to cause weight gain than older antidepressants like tricyclics or some SSRIs. In fact, some people lose a little weight early on due to nausea or reduced appetite. Long-term weight changes vary, but studies show minimal average gain - usually less than 2-3 pounds over a year. If weight gain becomes a problem, talk to your doctor about alternatives.
Is there a generic version of SNRIs?
Yes. Venlafaxine XR, desvenlafaxine, and duloxetine all have generic versions available in the U.S. Generic venlafaxine is one of the most prescribed antidepressants in the country. Prices vary, but generics typically cost $10-$30 per month with insurance, and under $20 without. This makes SNRIs more accessible than newer, brand-only options.
Can SNRIs be used for children?
Yes - but only one SNRI is FDA-approved for kids: duloxetine in its delayed-release granule form (Drizalma Sprinkle), approved for anxiety in children aged 7-17. Other SNRIs are used off-label in teens, but with caution. Doctors monitor growth, mood changes, and blood pressure closely in younger patients. Parents should watch for increased agitation or suicidal thoughts in the first few weeks.
Do SNRIs help with anxiety?
Yes. Duloxetine and venlafaxine are both FDA-approved for generalized anxiety disorder. Many patients report feeling calmer, less overwhelmed, and more able to focus after starting an SNRI. The norepinephrine boost helps reduce the physical symptoms of anxiety - like racing heart, muscle tension, and restlessness - which SSRIs sometimes don’t address as well.
What should I do if SNRIs don’t work?
If you’ve tried one SNRI at a full dose for 12 weeks and still don’t feel better, your doctor may switch you to another SNRI, try an SSRI, or consider non-antidepressant options like bupropion, mirtazapine, or even newer treatments like ketamine therapy. About 30-40% of depression cases don’t respond to any single medication - that doesn’t mean you’re hopeless. It means you need a different strategy. Work with your provider to explore combinations, therapy, or lifestyle changes.