Spinal Cord Injury: Understanding Function Loss, Rehabilitation, and Assistive Devices

When your spinal cord is injured, it’s not just about losing movement or feeling. It’s about losing control over your body in ways you never imagined-how you sit, breathe, go to the bathroom, or even hold a cup of coffee. Every year, nearly 18,000 people in the U.S. face this reality after a car crash, a fall, or an act of violence. For many, the road ahead isn’t about a full cure, but about rebuilding a life with new tools, new routines, and new support.
What Happens When the Spinal Cord Is Damaged?
The spinal cord is your body’s main communication line between your brain and everything below your neck. When it’s damaged, signals get blocked. The higher the injury, the more of your body is affected. A C1-C4 injury can leave you unable to breathe without a ventilator. A T12 injury might mean you lose leg movement but keep full arm function. And it’s not just muscles that go quiet-your bladder, bowels, blood pressure, and even your ability to sweat can stop working normally.Not all injuries are the same. Incomplete injuries mean some signals still get through. About 59% of people with incomplete paraplegia regain some ability to walk with training. Complete injuries mean no signals pass below the injury. Only 1-3% of those with complete paraplegia ever walk again without help. That’s why rehab starts the moment you’re stable-sometimes within 24 hours.
Rehabilitation Starts the Day You’re Stable
Rehab isn’t something you do later. It begins in the hospital, right after you’re out of danger. The goal? Stop new problems from forming and start rebuilding what you can. In the first few weeks, therapists focus on keeping your joints flexible. If you’re not moving your arms or legs, they move them for you-passive range-of-motion exercises-at least once a day, more if you have muscle spasms. Skip this, and your muscles and tendons tighten up, making movement harder later.Therapy isn’t just about stretching. You’ll get help with breathing-especially if your injury is high up. Techniques like assisted coughing, chest percussion, and incentive spirometry cut pneumonia risk by 65%. That’s huge. One study showed people using these methods stayed out of the hospital longer and recovered faster.
By the second or third week, you start learning how to transfer from bed to wheelchair, how to sit up without falling, and how to manage your bladder and bowels. That last part takes time-45 to 90 minutes a day, every day. It’s not glamorous, but it’s essential. And it’s not something you can do alone. Caregivers need training too. Poor transfer techniques cause 32% of shoulder injuries in family members who help you move.
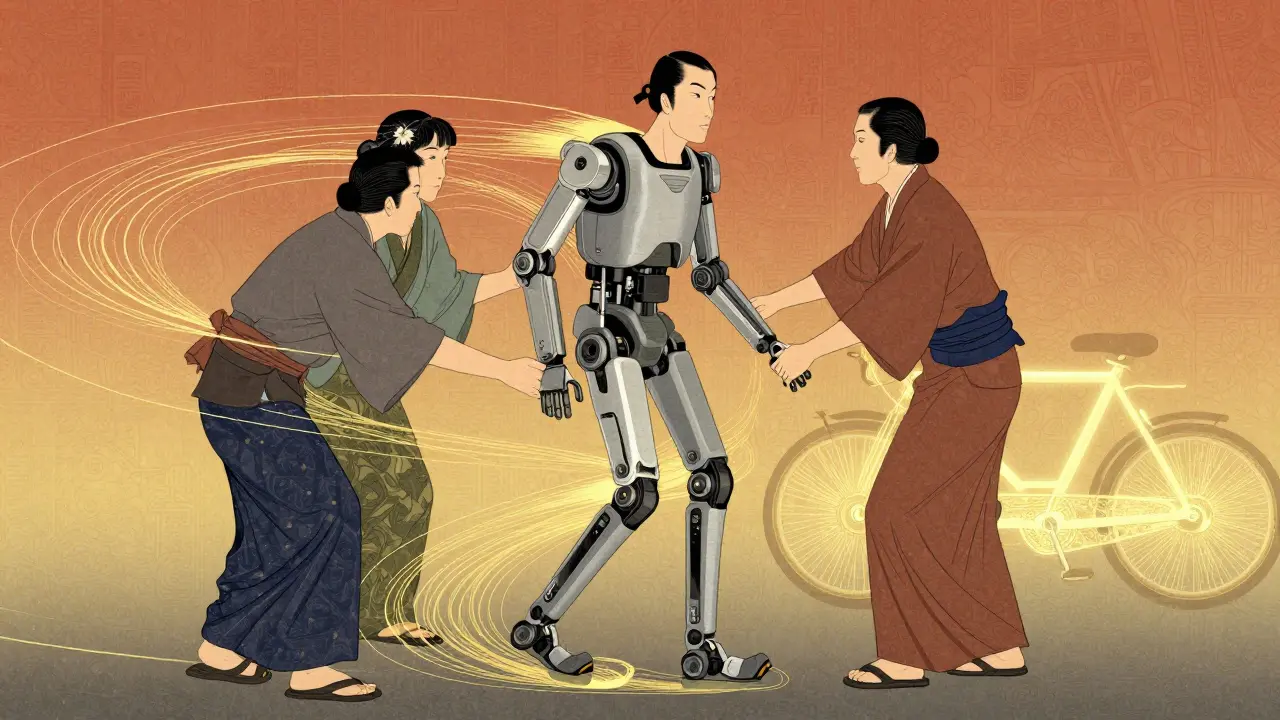
Advanced Tools That Help You Move Again
Modern rehab isn’t just about weights and treadmills. It’s using machines that literally help your body move. Functional Electrical Stimulation (FES) bikes send tiny electric pulses to your leg muscles, making them contract and pedal. People using FES bikes see a 14.3% boost in heart and lung capacity-far more than regular arm cycling. One user on a support forum said FES helped him keep his leg muscles from wasting away after a T6 injury, but the $5,000 cost for a home unit was too much to afford.Then there are exoskeletons. Devices like Ekso and ReWalk let people with paraplegia stand and take steps. One Reddit user shared that after three years without walking, his first steps in an Ekso exoskeleton felt like magic. But here’s the catch: each session lasts only 25 to 45 minutes. You need three therapists to help you safely. And insurance? Medicare only covers 80% of wheelchair costs-and even less for these high-tech devices. Out-of-pocket expenses for a custom seating system can hit $3,500.
For upper limbs, robotic arms like Armeo help people with cervical injuries practice reaching, grabbing, and lifting. These aren’t toys-they’re precision tools. And they’re becoming more common. By 2025, two-thirds of top rehab centers will use AI to adjust therapy plans based on your progress in real time.
Spasticity, Pain, and the Hidden Struggles
You might think the biggest challenge is walking. But for 65 to 78% of people with SCI, it’s spasticity-muscles that lock up, cramp, or kick out randomly. It can hurt. It can ruin sleep. It can make transfers impossible. Doctors manage it with a mix of pills like baclofen and injections of botulinum toxin. Studies show this combo reduces spasticity scores by 40-60% in nearly 8 out of 10 people.But pain doesn’t always come from muscles. Some feel burning, tingling, or electric shocks that never go away. That’s neuropathic pain. It doesn’t respond to regular painkillers. It needs special meds like gabapentin or antidepressants. And it’s often ignored in early rehab because it’s harder to measure than mobility.
Then there’s motivation. A survey found 68% of people quit their home exercise programs within six months. Why? No one’s checking in. No one’s celebrating small wins. Peer support makes a huge difference. At Spaulding Rehabilitation, 82% of patients said talking to someone who’d been through the same thing helped them adjust more than any therapy session.

Life After Rehab: What Comes Next?
Rehab doesn’t end when you leave the center. It just changes. Outpatient therapy drops to two or three sessions a week. You start learning to navigate the world-with ramps, accessible bathrooms, and adaptive vehicles. Many get powered wheelchairs with joystick controls or voice-activated systems. Some use smart home tech to turn on lights or open doors without lifting a finger.But access isn’t equal. Only 32% of general hospitals offer full SCI rehab programs. Most people go to one of the 17 specialized Model System centers. These places have teams of neuropsychologists, social workers, and therapists who work together daily. They don’t just hand you a pamphlet-they give you a 100+ page personalized plan. Other places? You get a one-page handout and a referral.
Insurance is another wall. Medicare pays only 83% of what it actually costs to run these programs. That’s why centers are turning to telehealth. Now, you can do check-ins, therapy reminders, and even virtual group sessions from your living room. That’s growing fast-73% of top centers now offer it.
The Future Is Here, But It’s Not Perfect
New tech is coming fast. In 2022, the FDA approved the first implantable device that stimulates the diaphragm-letting people with C3-C5 injuries breathe without a ventilator 74% of the time. That’s life-changing. And brain-computer interfaces? Early trials show people with cervical injuries can move a robotic hand with their thoughts, improving hand function by 38%. It’s not ready for everyone yet, but it’s real.Still, most of these tools are expensive, hard to access, and lack long-term data. Only 37% of studies track patients beyond six months. That’s a problem. We don’t know if exoskeletons help you live better over 10 years-or if they just make you tired.
One thing’s certain: the number of SCI cases is rising, especially in older adults. Falls are up 4.2% every year for people over 65. Our healthcare system isn’t ready for that. We need more rehab centers, better insurance rules, and more support for families. Because recovery isn’t just about walking again. It’s about living fully-with dignity, independence, and the tools to do it.
Can you walk again after a spinal cord injury?
It depends on whether the injury is complete or incomplete. About 59% of people with incomplete injuries regain some walking ability with intensive rehab. For complete injuries, only 1-3% regain the ability to walk independently. Technologies like exoskeletons and FES can help people stand and take steps, but they don’t restore natural walking. Progress is measured in small gains-not a return to how things were before.
How long does spinal cord injury rehab last?
Rehab happens in phases. The acute phase starts within 24-72 hours and lasts up to 12 weeks, focusing on preventing complications and learning basics like transfers and breathing. The subacute phase continues with more active training. Most people transition to outpatient care at 3-6 months, but improvement can continue for years. The first year is the most critical-you can regain 80-90% of your potential function if you’re consistent.
What assistive devices are most helpful for SCI?
It depends on the injury level. For lower-body injuries, powered wheelchairs, exoskeletons (like Ekso or ReWalk), and FES bikes help with mobility. For upper-body injuries, robotic arms (like Armeo) and voice-controlled smart home systems improve independence. For breathing issues, diaphragm pacing systems are life-changing. And for daily tasks, adaptive utensils, reachers, and bathroom aids are essential. The best device is the one that fits your life and goals.
Is spinal cord injury rehab covered by insurance?
Medicare and most private insurers cover inpatient rehab if you meet criteria-like needing 3 hours of therapy daily. But coverage for advanced devices like exoskeletons or FES bikes is spotty. Medicare covers 80% of wheelchair costs after your deductible, but you’re on the hook for the rest. Home FES units can cost $5,000 out-of-pocket. Many people can’t afford them. Insurance policies vary widely, and appeals are often needed.
What’s the biggest challenge after spinal cord injury?
It’s not just physical. While mobility and bladder control are hard, the biggest hurdle is emotional adjustment and isolation. Many people quit home exercises because they feel alone. Peer support programs cut that risk dramatically-82% of users say talking to someone who’s been through it helped them stay motivated. Finding community, whether online or in person, is often more important than any machine or therapy.
Oladeji Omobolaji
January 22, 2026 AT 22:44Man, this hit different. Back home in Lagos, folks with SCI just get left behind. No rehab, no devices, just prayers and family holding them up. I wish we had half the resources you guys do.
Anna Pryde-Smith
January 23, 2026 AT 04:35Y’ALL AREN’T TALKING ABOUT THE REAL ISSUE - THE SYSTEM IS DESIGNED TO MAKE YOU FEEL BROKE AND BROKEN. I SPENT 18 MONTHS FIGHTING INSURANCE JUST TO GET A NEW WHEELCHAIR. THEY WANT YOU TO JUST ‘ADJUST’ WHILE THEY PROFIT OFF YOUR SUFFERING.
Susannah Green
January 24, 2026 AT 04:45For anyone struggling with spasticity - baclofen + Botox combo works, but don’t skip the PT. I had 80% reduction in spasms after 6 weeks of daily stretching + nightly magnesium. Also, cold packs before bed? Game-changer. Seriously.
Vanessa Barber
January 25, 2026 AT 13:41‘Only 1-3% walk again’? Yeah, and I bet those numbers are cherry-picked from people who had perfect rehab. My cousin walked again after a T10 - no exoskeleton, just stubbornness and a treadmill. Numbers don’t tell the whole story.
dana torgersen
January 26, 2026 AT 10:28It’s… not… just… about… mobility… is… it?… The… silence… after… the… injury… the… way… people… look… through… you… like… you’re… a… ghost… with… a… wheelchair…
Dawson Taylor
January 28, 2026 AT 05:44The data on long-term functional outcomes remains critically insufficient. The majority of longitudinal studies terminate at six months, precluding robust conclusions regarding sustainability of gains from high-cost interventions such as exoskeletons and FES.
Laura Rice
January 28, 2026 AT 14:42My sister got her first FES bike last year. She cried the first time she pedaled. Not because she could move her legs - because she felt… alive. That’s the thing no study measures. The joy. The tiny rebellions against despair.
Andrew Smirnykh
January 29, 2026 AT 20:49I’m from Kenya, and I’ve seen how tech like this is either luxury or unattainable. In places without Medicare or private insurance, rehab is just ‘don’t get bedsores.’ Maybe the real innovation isn’t the machine - it’s making care a human right, not a privilege.
Kerry Moore
January 31, 2026 AT 05:02I appreciate the thoroughness of this post. The emphasis on peer support as a therapeutic modality is particularly compelling. The 82% statistic regarding emotional adjustment through lived-experience connection merits further institutional integration.
charley lopez
January 31, 2026 AT 05:27Functional Electrical Stimulation (FES) induces neuromuscular activation via controlled depolarization of motor nerves. The observed 14.3% increase in cardiopulmonary capacity is statistically significant (p<0.01) in controlled trials, and correlates with reduced secondary complications such as osteoporosis and pressure ulcers.
Kerry Evans
February 1, 2026 AT 13:15You people act like this is some kind of medical miracle. Newsflash: 90% of us will never walk again. And the ‘hope’ you’re selling? It’s just another way for corporations to sell $5000 bikes to people who can’t afford insulin. Stop romanticizing survival.
Sallie Jane Barnes
February 3, 2026 AT 08:36To the person who said ‘it’s not about walking’ - you’re right. It’s about dignity. It’s about being seen. I’ve been in rehab for two years. The day my therapist said, ‘What do you want to do?’ - not ‘What can you do?’ - that’s when I started living again.