Swollen Legs: Causes, Risks & Effective Treatments

Swollen Legs Risk Assessment Tool
Answer the following questions to assess your risk level for complications from swollen legs:
Your risk assessment will appear here after answering the questions above.
When swollen legs appear larger, tight, or puffy due to fluid buildup in the lower limbs, the issue can be anything from a short‑term annoyance to a sign of a serious health problem. Knowing why the swelling happens, what could go wrong if it’s ignored, and how to act can save you discomfort and prevent dangerous complications.
Key Takeaways
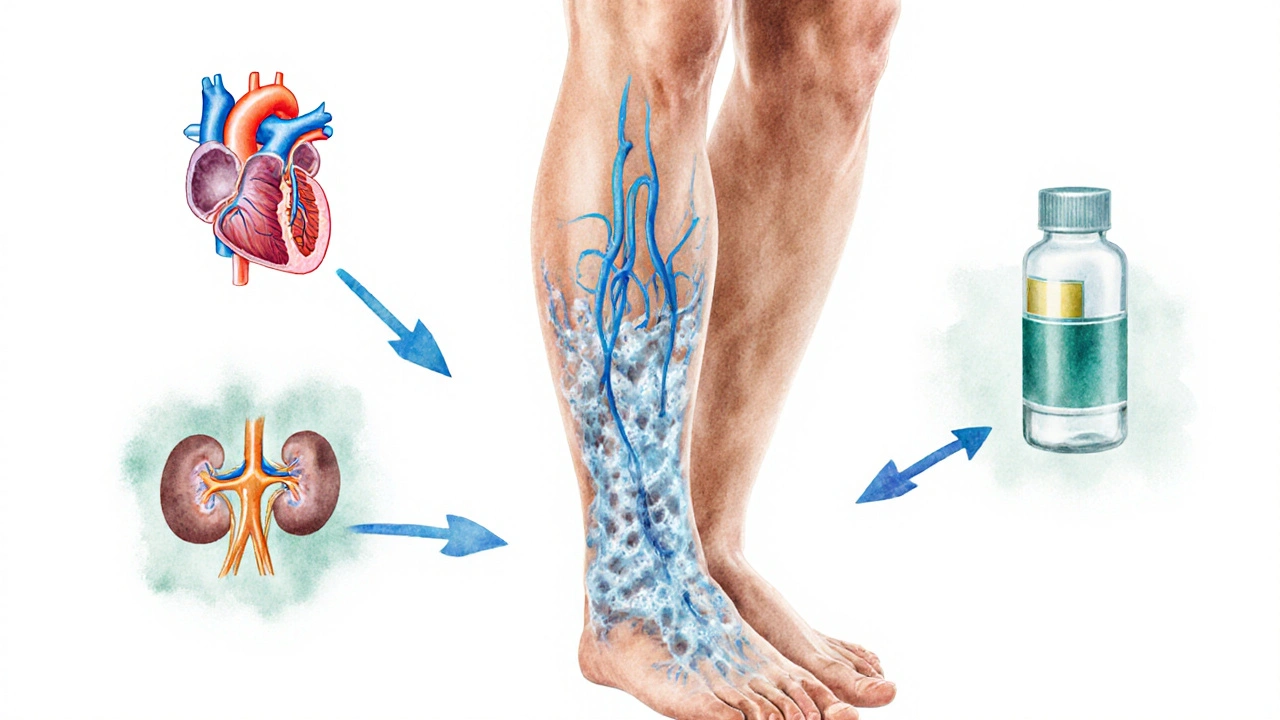
- Swelling (edema) often stems from vascular, cardiac, renal, medication‑related, or lifestyle factors.
- Complications include deep vein thrombosis, skin ulcers, and loss of mobility.
- Simple self‑care steps-elevation, compression, low‑salt diet-help many cases.
- Persistent or painful swelling warrants a medical evaluation for conditions like heart failure or chronic venous insufficiency.
- Early detection and targeted treatment dramatically lower the risk of long‑term damage.
What Exactly Is Swelling?
In medical terms, the swelling of the lower limbs is called edema an excess accumulation of fluid in the interstitial spaces of tissues. Gravity naturally pulls fluid down toward the feet, but the circulatory and lymphatic systems normally push it back up. When those pumps slow down or leak, fluid pools and the legs look puffier.
Major Causes-What Triggers the Fluid Buildup?
Understanding the root cause is key because each source needs a different fix. Below are the five most common categories.
1. Vascular Problems
Issues with veins or arteries disrupt normal blood flow. The two biggest culprits are:
- Chronic Venous Insufficiency (CVI): Vein valves become weak, allowing blood to pool. Over time, the pressure pushes fluid into surrounding tissue.
- Deep Vein Thrombosis (DVT): A clot forms in a deep thigh or calf vein, partially blocking return flow and causing sudden, often painful swelling.
Both conditions are linked to a higher risk of skin changes and ulcers if left untreated.
2. Cardiac Causes
When the heart can’t pump efficiently, blood backs up into the veins of the legs. Heart failure a condition where the heart’s pumping ability is reduced, leading to fluid retention is a classic example. Patients often notice swelling in the evenings that eases after a night of lying flat.
3. Renal (Kidney) Issues
The kidneys regulate fluid balance by filtering blood. Kidney disease any condition that impairs the kidneys’ ability to remove excess fluid and waste leads to systemic retention, which frequently shows up first in the ankles and calves.
4. Medication‑Induced Edema
Some drugs interfere with fluid regulation. Common offenders include:
- Non‑steroidal anti‑inflammatory drugs (NSAIDs pain relievers that can cause sodium retention)
- Calcium channel blockers used for hypertension
- Corticosteroids
If you start a new medication and notice swelling within a few weeks, ask your prescriber whether it’s a side effect.
5. Lifestyle Factors
Simple habits can aggravate fluid pooling:
- Prolonged standing or sitting without moving (common in office jobs and long flights)
- High‑salt diet, which forces the body to hold onto water
- Obesity, which adds pressure on veins and lymphatics
Addressing these habits often reduces mild swelling without medication.
Complications: Why Swelling Can Be Dangerous
If you ignore persistent swelling, several serious problems can develop.
- Deep Vein Thrombosis: A clot can break loose and travel to the lungs, causing a potentially fatal pulmonary embolism.
- Venous Stasis Ulcers: Chronic pressure damages skin, leading to painful open sores that heal slowly.
- Lymphedema: Over time, the lymphatic system can become overwhelmed, causing thickened, fibrotic tissue.
- Reduced Mobility: Swelling limits range of motion, increasing fall risk, especially in older adults.
Early detection and treatment dramatically cut the odds of these outcomes.
How Doctors Diagnose the Underlying Issue
When you seek care, a clinician will typically follow these steps:
- Medical history review - looking for heart, kidney, or medication clues.
- Physical exam - checking for pitting edema, skin changes, and temperature differences.
- Duplex ultrasound - visualizes blood flow and spots clots or valve incompetence.
- Blood tests - assess kidney function (creatinine, eGFR), heart markers (BNP), and electrolytes.
- Additional imaging - X‑ray or CT if deeper structural problems are suspected.
These tests help pinpoint whether the cause is vascular, cardiac, renal, medication‑related, or lifestyle‑driven.
Treatment Options: From Home Remedies to Medical Interventions
Effective management usually blends self‑care with professional treatment.
Self‑Care Strategies
- Elevation: Raise legs above heart level for 15‑20 minutes, three times daily. This uses gravity to push fluid back toward the torso.
- Compression: Wear compression stockings elastic garments that apply graduated pressure, helping veins move blood upward. Choose the appropriate compression level (15‑20mmHg for mild, 20‑30mmHg for moderate cases).
- Exercise: Simple calf‑pump actions - like ankle circles or marching in place - engage the muscle pump that returns blood.
- Low‑Salt Diet: Aim for <2,300mg sodium per day; more stringent (1,500mg) if heart or kidney disease is present.
- Hydration: Drinking enough water prevents the body from retaining excess fluid as a defense mechanism.
Medical Treatments
- Diuretics: Medications that increase urine output, commonly prescribed for heart or kidney‑related edema.
- Venous Procedures: Endovenous laser therapy or sclerotherapy to close faulty veins in CVI.
- Anticoagulation: Blood thinners for DVT to prevent clot extension and pulmonary embolism.
- Lymphedema Therapy: Manual lymphatic drainage and specialized compression garments.
Always discuss medication changes with a healthcare professional; abrupt stops can worsen symptoms.

Prevention: Keeping Your Legs Light and Healthy
Prevention is about reducing the pressure on your circulatory and lymphatic systems.
- Move every hour - stand, stretch, or walk for a few minutes if you have a desk job.
- Maintain a healthy weight; a BMI under 25 lowers venous pressure.
- Limit alcohol; excessive intake can worsen liver‑related fluid retention.
- Check medication side‑effects regularly with your pharmacist.
Integrating these habits can keep mild swelling at bay and support overall vascular health.
When to Call a Doctor Immediately
Some red‑flag symptoms demand urgent attention:
- Sudden, severe swelling in one leg, especially with pain or warmth.
- Shortness of breath, chest pain, or rapid heartbeat alongside leg swelling.
- Swelling accompanied by a fever, redness, or foul‑smelling discharge.
- Swelling that doesn’t improve with elevation after 24‑48hours.
Prompt evaluation can prevent life‑threatening complications like pulmonary embolism or severe infection.
Quick Recap
Swelling isn’t just cosmetic-it’s a window into how well your heart, kidneys, veins, and lymphatics are working. By spotting the cause early, you can apply the right mix of lifestyle tweaks and medical care to stay mobile and pain‑free.
| Cause Category | Typical Signs | Key Tests | First‑Line Treatment |
|---|---|---|---|
| Vascular (CVI, DVT) | Pitting edema, skin discoloration, calf pain | Duplex ultrasound, D‑dimer | Compression, anticoagulation (if DVT) |
| Cardiac (Heart Failure) | Leg swelling worsens at night, shortness of breath | Echocardiogram, BNP level | Diuretics, lifestyle modification |
| Renal (Kidney Disease) | Swelling in ankles, foamy urine, fatigue | Serum creatinine, eGFR | Fluid restriction, dialysis if advanced |
| Medication‑Induced | Onset after starting new drug, generalized edema | Review medication list, serum electrolytes | Switch drug, add diuretic if needed |
| Lifestyle | Swelling improves with rest, worsens after long sitting | Clinical exam, no special test | Elevation, regular movement, low‑salt diet |
Frequently Asked Questions
Why do my legs swell more in the evenings?
Gravity pulls fluid down while you’re upright. By the end of the day, the calf muscle pump gets tired, allowing fluid to pool. Elevating your legs at night helps reverse this process.
Can I treat swollen legs without seeing a doctor?
Mild, occasional swelling often improves with home measures-elevation, compression stockings, and reduced sodium. However, if swelling is sudden, painful, or accompanied by shortness of breath, seek medical attention promptly.
What’s the difference between edema and lymphedema?
Edema is a broad term for any fluid buildup, usually due to vascular or systemic issues. Lymphedema specifically results from a blocked lymphatic system, leading to a thick, fibrotic swelling that often feels heavier and may be resistant to standard compression.
Are compression stockings safe for everyone?
Most people can wear them, but those with severe arterial disease, peripheral neuropathy, or uncontrolled diabetes should get a doctor's clearance first, as excessive pressure could worsen circulation.
How much sodium is too much for preventing leg swelling?
The general recommendation is under 2,300mg per day. If you have heart or kidney disease, aim for 1,500mg or less. Reading food labels and avoiding processed snacks make this achievable.
Swollen legs are more than a cosmetic concern; they’re a signal from your body that something needs attention. By recognizing the cause, addressing complications early, and applying targeted treatments, you can keep your legs feeling light and healthy.
Rex Peterson
October 5, 2025 AT 14:45One might contemplate that edema of the lower limbs is not merely a superficial inconvenience but a manifestation of systemic equilibrium disturbance. Venous insufficiency, renal dysfunction, and cardiac failure each perturb hydrostatic pressures, prompting interstitial fluid accumulation. While the interactive tool offers a structured assessment, clinicians must also consider patient history and comorbidities. In sum, thoughtful analysis transcends a simplistic questionnaire.
Candace Jones
October 7, 2025 AT 11:12Great point about the broader clinical picture. If you’re tracking swelling, make sure to log any changes in pain or color, as those can signal complications. Staying proactive with the tool can help catch issues early.
Robert Ortega
October 9, 2025 AT 07:38From a neutral standpoint, it’s useful to remember that lifestyle factors like prolonged standing and high sodium intake can exacerbate leg edema. Incorporating gentle movement breaks during the day may mitigate fluid pooling. The assessment could benefit from a question about daily activity levels.
Elizabeth Nisbet
October 11, 2025 AT 04:05Exactly, those small habit tweaks can make a big difference. Encourage yourself to stretch every hour and keep hydrated – it’s a simple but effective coach tip.
Sydney Tammarine
October 13, 2025 AT 00:32Ah, the ever‑present drama of swollen limbs, a saga worthy of Shakespeare, yet reduced to a drab questionnaire! One must ask, why do we accept such mechanistic reductionism? It’s as if the poor afflicted are expected to self‑diagnose through a digital oracle while genuine medical insight is banished to the shadows. The risk assessment tool, while neatly packaged, neglects the nuanced interplay of psychosocial stressors, dietary habits, and even socioeconomic status. Have we considered that a person’s access to fresh produce, or the very shoes they are forced to wear, can directly influence lymphatic flow? Moreover, the binary “yes/no” format strips away the gradations of pain-pain is not a switch but a spectrum, fading in intensity or flaring like a tempest. 🚨 Let us not forget the hidden perils of complacency: chronic edema can precipitate cellulitis, deep vein thrombosis, or even ulceration, outcomes that no simple score can encapsulate. In the grand tapestry of health, this tool is but a single, flimsy thread. 🙄
josue rosa
October 14, 2025 AT 20:58Indeed, the reductionist design of the assessment appears to lack the requisite pathophysiological granularity. From a hemodynamic perspective, the interplay between venous return, capillary oncotic pressure, and interstitial compliance is oversimplified in a binary schema. Incorporating parameters such as serum albumin levels, eGFR, and even ankle‑brachial index could enhance predictive validity. Furthermore, the algorithm’s weighting schema does not reflect the differential risk magnitude associated with, for instance, chronic heart failure versus transient orthopedic immobilization. A multidimensional scoring matrix, possibly employing logistic regression coefficients derived from epidemiological cohorts, would provide a more robust risk stratification. Finally, the interface should permit longitudinal data entry to capture the temporal evolution of edema, thereby facilitating dynamic risk recalibration.
Shawn Simms
October 16, 2025 AT 17:25While the previous comments are well‑intentioned, the prose suffers from unnecessary verbosity and occasional grammatical slip‑ups. For example, “interstitial compliance is oversimplified in a binary schema” could be streamlined to “the binary schema oversimplifies interstitial compliance.” Conciseness would aid readability without sacrificing technical accuracy. Additionally, ensure consistent capitalization of abbreviations such as “eGFR” and avoid redundant commas. Precision in language mirrors precision in clinical assessment.
Geneva Angeles
October 18, 2025 AT 13:52Let’s look on the bright side-using this tool can actually empower patients to take charge of their health journey. By answering a few simple questions, they become more aware of the factors that could be worsening their swelling, such as medication side effects or hidden heart issues. This self‑awareness often sparks lifestyle changes, like reducing salt intake or incorporating leg‑elevating routines, which can dramatically improve outcomes. Moreover, the visual feedback of a risk score can motivate adherence to follow‑up appointments and prescribed therapies. In short, it’s a catalyst for proactive health management, turning passive sufferers into active participants.
Scott Shubitz
October 20, 2025 AT 10:18Ah, the optimism epidemic! Let’s not pretend this tool is some panacea. It’s riddled with superficiality, masking the gritty reality that many users will ignore the advice anyway until a crisis hits. The colorful interface may distract from the fact that without proper medical oversight, a self‑assigned risk level could lead to false security or needless panic. In other words, don’t let the pretty graphics lull you into complacency; real health decisions demand more than a click.
Soumen Bhowmic
October 22, 2025 AT 06:45Use the tool wisely and stay informed.