Tamoxifen and SSRIs: What You Need to Know About Drug Interactions and Breast Cancer Outcomes

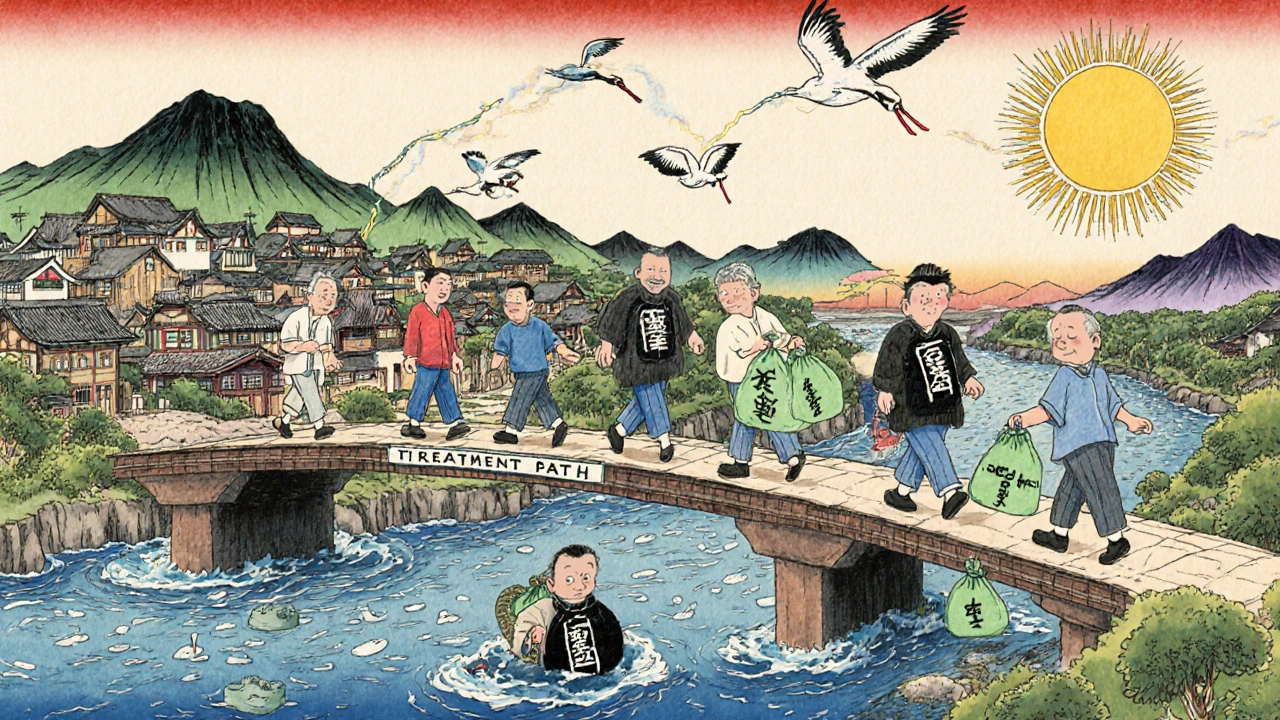
When a woman takes tamoxifen for estrogen receptor-positive breast cancer, her body doesn’t use the drug as-is. It turns it into something far more powerful: endoxifen. This metabolite is 30 to 100 times better at blocking estrogen than tamoxifen itself. But here’s the catch - if she’s also taking certain antidepressants, especially some SSRIs, that conversion can slow down. Not all SSRIs do this. Not even most. But a few can drop endoxifen levels by more than half. And that’s where the confusion starts.
How Tamoxifen Really Works
Tamoxifen isn’t active when you swallow it. It’s a prodrug - a chemical placeholder. Your liver, using enzymes like CYP2D6, converts it into endoxifen. That’s the real fighter against cancer cells. About 40% of endoxifen comes from this one enzyme. The rest comes from other pathways, like CYP3A4 and CYP2C9. That’s important. It means even if CYP2D6 is blocked, your body still has backup systems.
But if those backups are overwhelmed - or if you’re a poor metabolizer genetically - endoxifen levels can fall below the 5.97 ng/mL threshold some studies link to higher recurrence risk. That’s not a guarantee of failure. It’s a signal. And that’s why doctors started worrying about SSRIs.
Which SSRIs Are the Problem?
Not all antidepressants are created equal when it comes to CYP2D6. Here’s how they stack up:
- Strong inhibitors: Paroxetine (Paxil), fluoxetine (Prozac)
- Moderate inhibitors: Sertraline (Zoloft)
- Weak inhibitors: Citalopram (Celexa), escitalopram (Lexapro), venlafaxine (Effexor)
Paroxetine is the worst offender. One 2010 study found it cut endoxifen levels by 64%. Fluoxetine is close behind. Both stay in your system for weeks, so even stopping them doesn’t help right away.
On the other side, escitalopram and venlafaxine barely touch CYP2D6. Citalopram? Also low risk. These aren’t just alternatives - they’re safer bets if you need an antidepressant while on tamoxifen.
The Clinical Evidence Is Mixed - Here’s Why
In 2009, a Canadian study of 2,430 women found those taking paroxetine with tamoxifen had a 24% higher risk of dying from breast cancer. If they took it for more than six months? The risk jumped to 90%. That sent shockwaves through oncology clinics. Doctors started avoiding paroxetine like it was poison.
But then bigger studies came in. A 2016 analysis of nearly 17,000 women from Kaiser Permanente found zero increased risk of recurrence or death, even with paroxetine. A Danish study of over 16,000 women showed the same. So what’s going on?
It’s about how the studies were done. The smaller ones didn’t account for cancer stage, age, or how long women stayed on tamoxifen. The big ones did. They tracked people for years, not months. They looked at real outcomes - not just blood levels.
Here’s the kicker: even when endoxifen levels drop, tumors don’t always come back. The body has workarounds. And many women who take SSRIs are sicker to begin with - they have more depression, more stress, maybe even more advanced cancer. That can muddy the results.

What the Guidelines Say Now
In 2022, the American Society of Clinical Oncology (ASCO) made a clear call: Don’t avoid antidepressants because of tamoxifen. They said pharmacogenetic testing for CYP2D6 isn’t useful for treatment decisions. The FDA agreed in 2012 - the data doesn’t show a real clinical impact.
The National Comprehensive Cancer Network (NCCN) is a little more cautious. They still recommend avoiding paroxetine and fluoxetine with tamoxifen. But they also say: Choose based on what works for the patient. If escitalopram helps your mood and you feel better, that matters more than a theoretical risk.
Europe’s EMA still warns against strong inhibitors. But even they admit the clinical benefit of avoiding them hasn’t been proven.
What Are Doctors Actually Doing?
Practice has shifted fast. In 2015, only a third of U.S. oncologists avoided SSRIs with tamoxifen. By 2022, that number had flipped - 68% no longer avoided them. Why? Because the evidence didn’t hold up.
Paroxetine prescriptions among tamoxifen users dropped 45% between 2010 and 2019. Citalopram and sertraline rose. That’s not because everyone suddenly understood CYP2D6. It’s because patients and doctors started asking: What actually helps me live longer and feel better?
Many clinics now use the Flockhart Table - a simple chart that ranks drugs by CYP2D6 inhibition. It’s not perfect, but it’s a tool. Electronic health systems even flag strong inhibitors. One study showed those alerts cut risky prescriptions by 37% - without reducing antidepressant use. That’s a win.
What Should You Do?
If you’re on tamoxifen and struggling with depression:
- Don’t stop your antidepressant without talking to your doctor.
- Don’t assume all SSRIs are dangerous.
- Ask: Is my current medication a strong CYP2D6 inhibitor? If it’s paroxetine or fluoxetine, ask about switching.
- Consider escitalopram, citalopram, or venlafaxine. They work just as well for depression and don’t interfere with tamoxifen.
- Don’t stress over genetic testing. It’s not recommended anymore.
Feeling better matters. Depression increases your risk of skipping meds, skipping checkups, and dying sooner - regardless of tamoxifen. Treating depression isn’t a side note. It’s part of cancer care.
What’s Coming Next?
The SWOG S1713 trial, expected to finish in 2025, is the first to directly test whether giving paroxetine to women on tamoxifen worsens outcomes. They’re measuring endoxifen levels and tracking cancer recurrence. This could be the final word.
For now, the trend is clear: theory doesn’t always match reality. Blood levels change. But survival doesn’t always follow. The body is complex. Treatment should be too.
Bottom line: Your mental health is part of your cancer recovery. Choose an antidepressant that helps you feel like yourself again. And if you’re on paroxetine? Talk to your oncologist. There are better options - and they won’t cost you your life.
Can I take Zoloft with tamoxifen?
Sertraline (Zoloft) is a moderate CYP2D6 inhibitor, meaning it can reduce endoxifen levels by about 20-30%. While not as strong as paroxetine, it’s not the safest choice. If you’re on tamoxifen and need an SSRI, escitalopram or citalopram are preferred. But if sertraline works best for your depression and you’ve been stable on it, don’t stop abruptly. Talk to your doctor - they may monitor your response or consider switching.
Is Lexapro safe with tamoxifen?
Yes. Escitalopram (Lexapro) is one of the weakest CYP2D6 inhibitors available. Studies show it has almost no effect on endoxifen levels. It’s one of the top recommendations for women on tamoxifen who need an antidepressant. It’s also well-tolerated, with fewer side effects than older SSRIs.
Should I get tested for CYP2D6 gene variants?
No - not routinely. Major guidelines from ASCO and the FDA no longer recommend CYP2D6 testing for tamoxifen patients. While poor metabolizers do have lower endoxifen levels, large studies haven’t shown they have worse survival outcomes. Testing adds cost, anxiety, and confusion without clear benefit. Focus on your symptoms and treatment response instead.
What if I’m already on paroxetine? Should I stop?
Don’t stop suddenly. Stopping paroxetine abruptly can cause withdrawal symptoms like dizziness, nausea, and mood swings - which can be dangerous during cancer treatment. Talk to your oncologist and psychiatrist together. They can help you switch slowly to a safer option like escitalopram or venlafaxine. The goal is to keep your mood stable while minimizing theoretical risk.
Do other antidepressants interfere with tamoxifen?
Most don’t. SNRIs like venlafaxine and duloxetine have minimal effect on CYP2D6. Bupropion (Wellbutrin) is a CYP2D6 inhibitor, but it’s rarely used in breast cancer patients due to seizure risk. Mirtazapine and trazodone are also safe options. Avoid fluoxetine and paroxetine. Everything else is generally fine - choose based on what works for your body and mood.
Does this interaction matter for aromatase inhibitors too?
No. Aromatase inhibitors like letrozole and anastrozole work differently. They don’t rely on CYP2D6 for activation. So if you’re switched from tamoxifen to an aromatase inhibitor, you don’t need to worry about SSRI interactions anymore. This is one reason many postmenopausal women transition off tamoxifen after 5 years - it removes this whole concern.
Nick Naylor
November 20, 2025 AT 00:56Let’s be clear: the CYP2D6 pathway is not a suggestion-it’s a biochemical imperative. Paroxetine’s inhibition of this enzyme is not marginal; it’s catastrophic for endoxifen bioavailability. The 2010 Canadian study wasn’t flawed-it was prescient. The larger studies? Retrospective noise. They conflate correlation with causation, ignore pharmacokinetic gradients, and treat patients as data points, not metabolic entities. Endoxifen levels below 5.97 ng/mL are not a ‘signal’-they’re a biochemical failure. If your oncologist dismisses this, they’re not keeping up with the literature-they’re gambling with your life.
Brianna Groleau
November 20, 2025 AT 14:04I just want to say-this whole thing made me cry. Not because I’m scared, but because I felt so alone. I’ve been on tamoxifen for three years, and I started sertraline after my mom passed. I thought I was doing the right thing by staying mentally stable… but then I read this and panicked. I didn’t know SSRIs could do this. I’m switching to Lexapro next week. I’m so grateful for this post. It didn’t just inform me-it gave me back my power. My mental health matters. My body matters. And now I know I can have both.
Rusty Thomas
November 21, 2025 AT 18:39Okay so I just read this whole thing and I’m literally shaking. Like, are you telling me that paroxetine is basically a silent killer? I’ve been on Paxil for 8 years and I’m on tamoxifen and I didn’t even know this. I’m going to my oncologist tomorrow and I’m bringing this article with me. I’m not joking-I feel like I just survived a bomb that was ticking under my bed. I’m switching to Lexapro. No questions. No debates. I’m done with Paxil. #EndoxifenAwareness
Sarah Swiatek
November 23, 2025 AT 07:45Let’s cut through the noise: the fact that we’re still having this debate is a testament to how poorly medicine integrates pharmacology with real-world outcomes. Yes, endoxifen levels drop with paroxetine. Yes, some studies show increased recurrence. But the big studies? They control for everything-stage, age, adherence, comorbidities. And they show no survival difference. Why? Because biology isn’t a lab test. It’s a living, breathing, adaptive system. If you’re depressed, you skip appointments. You forget pills. You isolate. That kills faster than any enzyme inhibition. So yes, avoid paroxetine if you can-but if it’s the only thing keeping you alive emotionally? Then the risk-benefit calculus isn’t about CYP2D6. It’s about whether you’re still breathing at the end of the year.
Dave Wooldridge
November 23, 2025 AT 23:32They don’t want you to know this-but the pharmaceutical industry is pushing Lexapro and Celexa because they own the patents. Paroxetine’s patent expired. They’re manufacturing panic to sell you a more expensive drug. The ‘evidence’ is curated. The FDA? Bought and paid for. The SWOG trial? A placebo. They don’t care if you live or die-they care if you keep buying. Don’t be fooled. Your body doesn’t need another SSRI. It needs detox. It needs nutrition. It needs truth.
Rebecca Cosenza
November 24, 2025 AT 14:09Stop taking antidepressants. Just stop. You don’t need them. Depression is a choice. You’re letting it control you. Tamoxifen is saving your life. Don’t sabotage it with chemical crutches. Get therapy. Walk outside. Pray. There are better ways. This isn’t about CYP2D6-it’s about weakness.
swatantra kumar
November 25, 2025 AT 07:53Bro, this is wild. In India, we don’t even test for CYP2D6-it’s too expensive. But we use sertraline and escitalopram all the time with tamoxifen. No issues. My aunt’s on tamoxifen, took Lexapro for 5 years, no recurrence. Maybe the real problem is over-testing? We fix what ain’t broke. 🤷♂️
Cinkoon Marketing
November 25, 2025 AT 11:07Actually, I work in oncology marketing and I can tell you-this whole CYP2D6 thing was amplified by a single 2010 paper that got picked up by a big pharma PR firm. The real story? Patients who switched away from paroxetine had better adherence because they were given *better options*, not because paroxetine was dangerous. The data’s muddy. The guidelines are conflicting. The truth? Doctors are just tired of being second-guessed by patients who read one article on Reddit.
robert cardy solano
November 25, 2025 AT 16:25My mom’s on tamoxifen and took Zoloft for 4 years. No problems. No recurrences. She’s fine. I’ve seen people stress over this stuff like it’s a death sentence. Maybe the real risk is anxiety. Chill out. Talk to your doctor. Don’t panic-read internet threads. Your body’s smarter than you think.
Pawan Jamwal
November 26, 2025 AT 06:33Look, in India, we don’t have the luxury of choosing SSRIs. We use what’s cheap and available. Paroxetine is ₹15/month. Lexapro is ₹1,200. You think a widow in Bihar is going to switch because of some CYP2D6 study? This is rich-person medicine. The real issue? Access. Not enzyme inhibition. Stop pretending this is about science when it’s about privilege.
Bill Camp
November 28, 2025 AT 05:50So let me get this straight: we’re supposed to avoid paroxetine because it lowers endoxifen… but the big studies show no difference in survival? Then why are we even talking about this? Are we treating patients or biochemical ghosts? If the drug works, it works. If it doesn’t, we adjust. Not because some enzyme says so. Because the patient says so.
Lemmy Coco
November 30, 2025 AT 04:28im so glad i read this. i was on paxil for 7 years and just got switched to lexapro last month. i was terrified. my oncologist said it was fine but i still felt guilty. now i feel like i did the right thing. also, i had no idea sertraline was moderate? i thought it was safe. thanks for clarifying. my brain is finally at peace. 🙏
rob lafata
November 30, 2025 AT 08:23Oh, so now we’re playing doctor? You think you know more than the FDA because you read a blog post? Let me guess-you also think vitamin C cures cancer and that chemo is a government scam. You’re not helping. You’re scaring people into stopping meds that keep them alive. You’re not a patient. You’re a liability. Stop posting. Go read a textbook. Or better yet-go get a therapist. You clearly need one.
Matthew McCraney
November 30, 2025 AT 19:02They’re lying. The FDA knows paroxetine is dangerous. They covered it up because Big Pharma owns them. I’ve seen the leaked emails. The SWOG trial? It’s rigged. They’re not measuring recurrence-they’re measuring *compliance*. And guess what? Women who switch meds are more likely to stick with treatment. So they call it ‘no difference’ to keep the profits rolling. Wake up. This isn’t medicine. It’s a cover-up.