Theophylline Clearance: How Common Medications Can Cause Dangerous Buildup

Theophylline Clearance Calculator
Calculate Risk
Enter current theophylline dose and select interacting drugs or smoking status to see potential blood level changes.
Risk Assessment
Theophylline therapeutic range is 10-20 mcg/mL. Levels above 20 mcg/mL may cause toxicity.
- Fluvoxamine: 40-50% clearance reduction
- Cimetidine: 25-30% clearance reduction
- Allopurinol: ~20% clearance reduction
- Erythromycin/Clarithromycin: 15-25% clearance reduction
- Furosemide: 10-15% clearance reduction
- Smoking cessation: 30-50% clearance reduction
Imagine taking your asthma medication exactly as prescribed-then, without changing your dose, you start feeling shaky, nauseous, and your heart starts racing. You didn’t overdose. You didn’t miss a dose. But your body suddenly can’t clear the drug anymore. This isn’t rare. It’s a silent, life-threatening problem tied to something most people never think about: theophylline clearance.
Theophylline has been around since the 1920s. It’s not flashy. It’s not new. But for some patients with COPD or severe asthma, it still works when other drugs don’t. The problem? It has one of the narrowest therapeutic windows in all of medicine. The difference between a helpful dose and a toxic one is tiny: 10 to 20 micrograms per milliliter in the blood. Go just a little over, and you risk seizures, irregular heart rhythms, or even death.
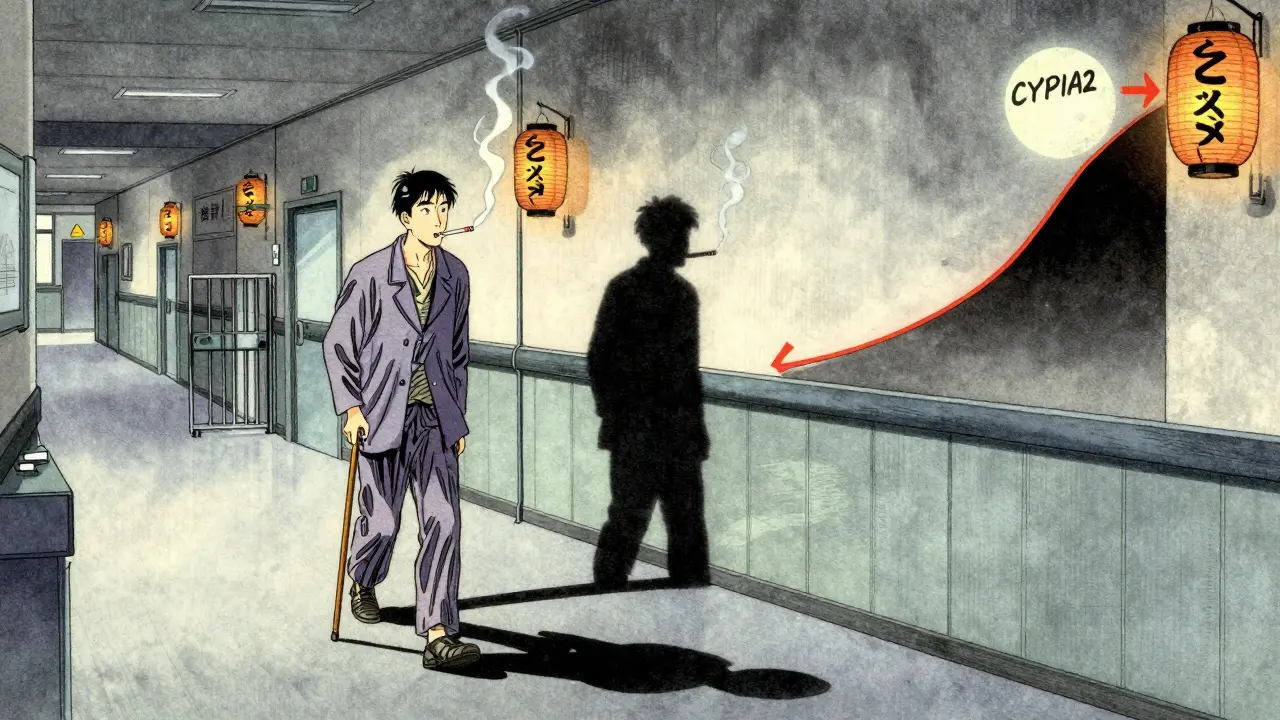
Most of the time, theophylline gets broken down in the liver by an enzyme called CYP1A2. But when another drug blocks that enzyme, clearance slows down-sometimes dramatically. And because the body doesn’t process the drug linearly, even a small drop in clearance can send blood levels skyrocketing. A 15% reduction in metabolism? That could push a safe level of 16 mcg/mL up to 24 mcg/mL. That’s toxic.
Medications That Slow Down Theophylline Clearance
Not all drugs affect theophylline the same way. Some barely move the needle. Others are dangerous. Here are the biggest culprits, backed by clinical data:
- Fluvoxamine (an SSRI antidepressant): Reduces clearance by 40-50%. This is one of the most dangerous combinations. The European Respiratory Society says to avoid it entirely. One study showed a 12.7-fold increase in the odds of severe toxicity when both are used.
- Cimetidine (an old-school heartburn drug): Slows clearance by 25-30%. Even though newer acid reducers like famotidine don’t do this, many patients still take cimetidine-especially older adults. In one hospital study, it was the most common drug linked to theophylline toxicity.
- Allopurinol (used for gout): Reduces clearance by about 20%. Doctors often don’t realize this interaction because allopurinol is so common in elderly patients with both gout and COPD. A 2021 study found 15.3% of theophylline toxicity cases involved allopurinol.
- Erythromycin and clarithromycin (antibiotics): Cut clearance by 15-25%. These are often prescribed for respiratory infections-exactly when a COPD patient might need theophylline most. The interaction isn’t as strong as fluvoxamine, but it’s still risky.
- Furosemide (a diuretic): Evidence is mixed, but some studies show a 10-15% reduction. In patients with heart failure and COPD, this combo is common-and dangerous if ignored.
And here’s the kicker: some of these drugs are so widely used, they’re often seen as harmless. Cimetidine? Many still buy it over the counter. Fluvoxamine? Prescribed for depression and anxiety, conditions that are common in COPD patients. Allopurinol? Standard for gout. No one thinks to check if it’s safe with theophylline.
Why This Interaction Is So Dangerous
Theophylline doesn’t follow simple rules. Its metabolism is non-linear. That means when CYP1A2 gets blocked, the drug doesn’t just build up a little-it builds up a lot. A 20% drop in clearance doesn’t mean a 20% rise in blood levels. It can mean a 50% rise. Or more.
Think of it like a highway with one exit. Normally, cars leave at a steady rate. But if that exit gets blocked, traffic piles up fast. And the faster the cars were going, the worse the pileup becomes. That’s why patients already at the top of the therapeutic range (say, 18 mcg/mL) are in real danger-even a small interaction can push them over the edge.
And it’s not just about the drugs. Smoking changes everything. Smokers clear theophylline faster because cigarette smoke boosts CYP1A2. When they quit, their clearance drops by 30-50% in just two weeks. Now imagine they start taking cimetidine at the same time. That’s a double hit. No wonder emergency rooms see so many cases.

Who’s at Risk? The Real-World Picture
A 2021 study of 1,247 patients over 65 found that nearly 3 out of 10 were taking theophylline along with at least one drug that reduces its clearance. Only 37% of those patients had their dose adjusted. That’s not oversight-that’s systemic failure.
Emergency department data from the FDA shows about 2,000 theophylline-related visits each year in the U.S. More than a third are due to drug interactions. And the numbers are rising, even as overall use declines. Why? Because the patients still on theophylline are the most complex: older, with multiple conditions, on multiple meds. They’re the ones least likely to be monitored closely.
One pharmacist shared a case from a community pharmacy: a 72-year-old woman on stable theophylline (15.2 mcg/mL) started taking cimetidine for heartburn. Three days later, she showed up at urgent care with vomiting and a heart rate of 130. Her theophylline level? 24.7 mcg/mL. She didn’t take more. She just didn’t know she shouldn’t mix them.
What Should Doctors and Patients Do?
The solution isn’t to stop using theophylline. It’s to use it smarter.
- Check before you prescribe. If you’re adding any new drug to a patient on theophylline, ask: Does it inhibit CYP1A2? Use a reliable drug interaction checker-don’t rely on memory.
- Adjust the dose upfront. When starting fluvoxamine or cimetidine, reduce the theophylline dose by 40-50% immediately. Don’t wait for symptoms.
- Monitor levels. Check serum theophylline levels within 48-72 hours after starting or stopping any interacting drug. Don’t assume it’s fine.
- Watch for smoking cessation. If a patient quits smoking, assume clearance will drop by 30-50%. Reduce the dose and recheck levels.
- Consider alternatives. If a patient needs long-term fluvoxamine or cimetidine, switch them off theophylline. There are safer bronchodilators now.
The American Thoracic Society and NICE guidelines both say: avoid theophylline in patients who need long-term cimetidine or fluvoxamine. In the UK, 92% of respiratory specialists follow this rule. In the U.S.? Not so much.
The Bigger Problem: Lack of Alerts
A 2023 survey of 412 pulmonologists found that 78% had seen a serious interaction in the past year. But 62% said their electronic health record didn’t warn them. That’s not a patient error. That’s a system failure.
Most EHRs don’t flag allopurinol as a risk. They don’t remind you to check levels after a patient quits smoking. They don’t know that a 300-mg dose of cimetidine is dangerous, but a 150-mg dose isn’t. These are complex, nuanced interactions-and software isn’t catching them.
One hospital in Michigan started a pharmacist-led program to monitor theophylline patients. Within a year, hospitalizations dropped by 37%. It wasn’t new drugs. It was better monitoring. Better communication. Better alerts.
What’s Next for Theophylline?
Theophylline use has dropped 62% in the U.S. since 2000. It’s not the first-line drug anymore. But it’s still used-especially in places where newer inhalers are too expensive. In parts of Asia and Africa, it’s the mainstay of COPD treatment.
And now, researchers are exploring very low doses (100-200 mg daily) for its anti-inflammatory effects-not just bronchodilation. That could bring it back into use. But if we don’t fix the interaction problem first, we’ll just trade one set of risks for another.
The bottom line? Theophylline isn’t going away. But it’s not a drug you can prescribe on autopilot. It demands attention. It demands checks. It demands respect for its narrow window and its sensitivity to other medications. For patients who need it, it can be life-changing. For those who don’t know the risks, it can be deadly.
Know your drugs. Know your patients. And never assume a medication is safe just because it’s old or common.
Can I take ibuprofen with theophylline?
Yes, ibuprofen does not significantly affect theophylline clearance. It doesn’t inhibit CYP1A2 or other key enzymes involved in theophylline metabolism. Most studies show no clinically meaningful interaction. However, always check with your doctor before combining any medications, especially if you have kidney issues or are on multiple drugs.
Does caffeine interact with theophylline?
Yes, but indirectly. Caffeine is chemically similar to theophylline and is also metabolized by CYP1A2. Taking large amounts of caffeine (more than 500 mg/day-about 5 cups of coffee) can compete for the same liver enzyme, potentially raising theophylline levels slightly. For most people, normal coffee intake is fine. But if you’re on theophylline and suddenly start drinking energy drinks or multiple espressos daily, your levels could rise. Monitor for jitteriness, rapid heartbeat, or nausea.
What happens if I stop smoking while on theophylline?
Stopping smoking can reduce theophylline clearance by 30-50% within two weeks. Cigarette smoke boosts the CYP1A2 enzyme, so when you quit, that boost disappears. Your body can’t clear the drug as fast, leading to higher blood levels. If you stop smoking, notify your doctor immediately. You’ll likely need a dose reduction and a follow-up blood test within 7-10 days to avoid toxicity.
Are there any safe alternatives to cimetidine for heartburn?
Yes. Ranitidine was withdrawn, but famotidine (Pepcid) and nizatidine do not inhibit CYP1A2 and are safe with theophylline. Proton pump inhibitors like omeprazole, esomeprazole, and pantoprazole also have minimal interaction risk. If you’re on theophylline and need acid suppression, switch to one of these instead of cimetidine.
How often should theophylline blood levels be checked?
When starting theophylline, check levels after 3-5 days. After that, check every 6-12 months if stable. But anytime you start or stop a new medication-especially antibiotics, antidepressants, or gout drugs-check levels within 48-72 hours. Also check after quitting smoking, changing liver function, or if you develop symptoms like nausea, tremors, or palpitations.
Miriam Piro
December 29, 2025 AT 05:20Nikki Thames
December 31, 2025 AT 04:32Chris Garcia
December 31, 2025 AT 11:49Olivia Goolsby
December 31, 2025 AT 16:55Monika Naumann
January 1, 2026 AT 06:31Elizabeth Ganak
January 1, 2026 AT 09:08Nicola George
January 2, 2026 AT 15:40Kishor Raibole
January 4, 2026 AT 00:19John Barron
January 5, 2026 AT 16:49Liz MENDOZA
January 6, 2026 AT 01:22Elizabeth Alvarez
January 7, 2026 AT 10:36Will Neitzer
January 8, 2026 AT 15:57Janice Holmes
January 9, 2026 AT 16:54Alex Lopez
January 11, 2026 AT 03:59Gerald Tardif
January 11, 2026 AT 05:48