UK NHS Substitution Laws Explained: 2025 Policy Changes & Real-World Impact

In 2025, the UK's National Health Service is overhauling how medications and healthcare services are delivered. These changes, driven by new laws, are reshaping everything from pharmacy operations to hospital care. For patients and healthcare workers, this means real shifts in how care is provided.
Understanding UK NHS substitution laws is key to navigating these changes. Substitution isn't just about swapping one drug for another-it's a complex system affecting where care happens, how it's delivered, and who pays for it. Let's break down what's changing and why it matters.
What UK Substitution Laws Really Mean
pharmaceutical substitution the process where pharmacists replace prescribed branded medicines with generic equivalents has been part of NHS practice for decades. It started with the Medicines Act 1968 but got updated by the NHS (Pharmaceutical Services) Regulations 2013. Now, the Human Medicines (Amendment) Regulations 2025 a major update to pharmaceutical service rules effective June 2025 has changed everything. These regulations require all NHS pharmaceutical services to be delivered remotely by Digital Service Providers (DSPs) pharmacy contractors operating without face-to-face consultations, removing traditional in-person pharmacy services.
Meanwhile, service substitution replacing hospital-based care with community or digital alternatives is happening across the NHS. The government's 2025 mandate explicitly says: "move care from hospital to community, sickness to prevention, and analogue to digital." This means shifting everything from routine check-ups to emergency follow-ups out of hospitals and into community settings or virtual platforms.
How Pharmaceutical Substitution Works Today
For medications, pharmacists can swap a branded drug for a cheaper generic version unless the doctor writes "dispense as written" (DAW) on the prescription. Before 2025, about 83% of eligible prescriptions used generics. The new regulations now require 90% generic substitution rates for all eligible medications. This change aims to save the NHS money while keeping quality high.
But there's a catch. The Human Medicines (Amendment) Regulations 2025 also removed tax credit exemptions for certain patients. Effective April 5, 2025, people who previously got free prescriptions due to tax credits now face charges for some medications. This affects low-income patients who relied on those exemptions.
Here's how the rules changed:
| Aspect | Pre-2025 | 2025 Reforms |
|---|---|---|
| Generic substitution rate | 83% average | 90% minimum requirement |
| Pharmacy service delivery | Face-to-face on premises | Remote dispensing only |
| New pharmacy applications | Market entry test applied | Pre-June 2025 applications under old rules |
| Tax credit exemptions | Available for prescription costs | Removed for NHS travel expenses |
Service Substitution: From Hospitals to Community Care
The NHS is moving care out of hospitals to save money and reduce waiting lists. For example, the government aims to cut emergency admissions for people over 65 by 15% by 2026-27. How? By replacing hospital visits with community-based support. This includes things like home-based care teams, community diagnostic hubs, and virtual consultations.
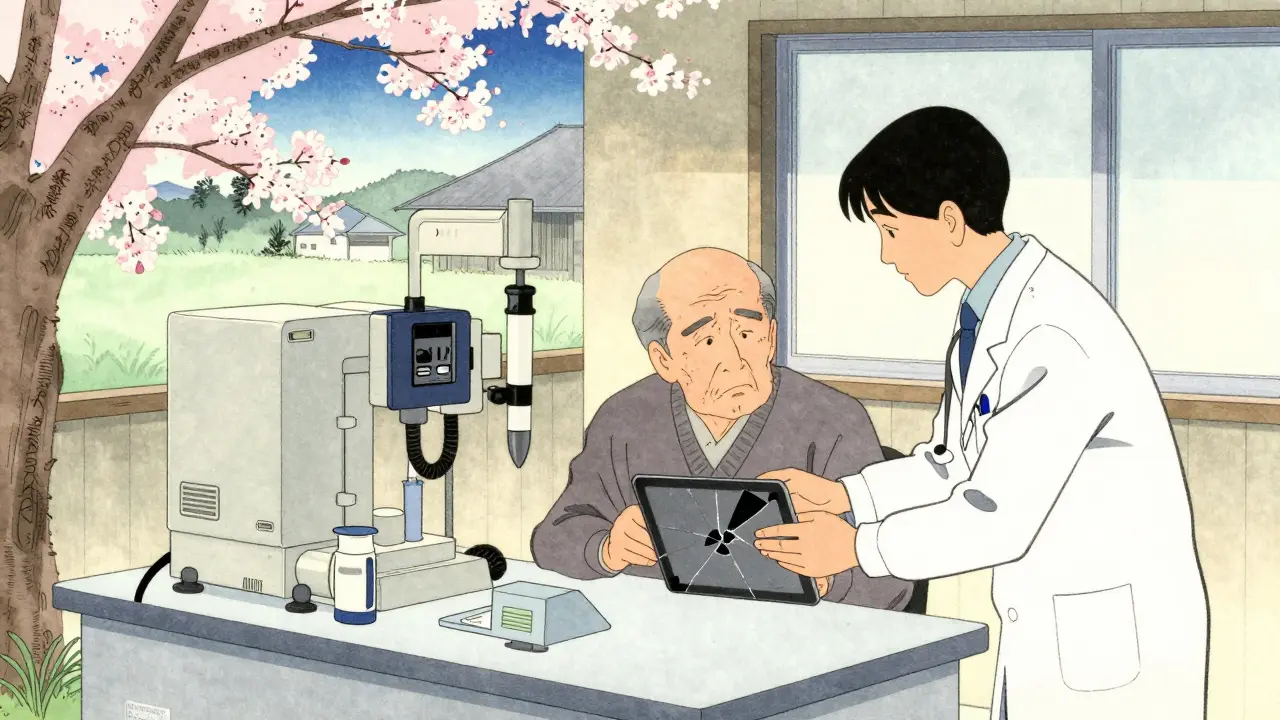
A real example: Manchester Royal Infirmary switched to virtual fracture clinics. This cut unnecessary follow-up appointments by 40%. But it also caused problems for 15% of elderly patients who couldn't use digital tools. "I had a broken wrist," shared one patient on Reddit, "but I couldn't do the video call because my tablet broke. I had to wait weeks for a physical appointment."
Community diagnostic hubs are replacing 22% of hospital-based diagnostic tests by 2027. These hubs do X-rays, blood tests, and scans in local centers instead of hospitals. The NHS allocated £650 million for this initiative. But 42% of rural trusts lack the infrastructure to support these hubs, according to the NHS Confederation's April 2025 report.
Real Challenges: Workforce Shortages and Patient Safety
The biggest problem with these changes? People. The NHS Confederation found 68% of Integrated Care Boards (ICBs) report not enough staff to handle the shift from hospitals to community care. Rural areas are hit hardest-42% of trusts there don't have the workforce or facilities needed.
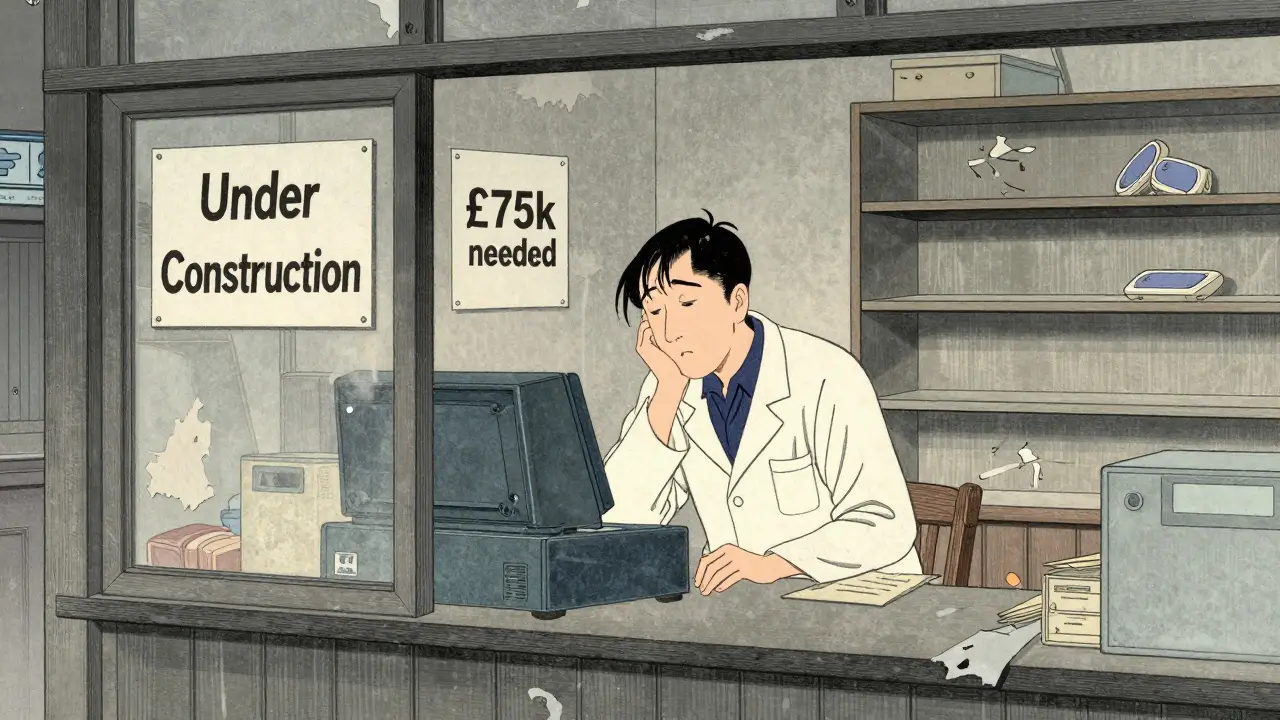
Pharmacies are struggling too. A British Pharmaceutical Industry survey in March 2025 showed 79% of community pharmacies worry about the remote dispensing rules. Half of them (54%) need £75,000-£120,000 to buy new technology. "We're a small town pharmacy," said one owner, "but we can't afford to replace our entire system overnight. What happens if we can't comply?"
Patient safety is also a concern. In North West London, a pilot program for remote dispensing saw a 12% increase in medication errors. Dr. Sarah Wollaston, former Chair of the Health and Social Care Committee, warned in the British Medical Journal: "The current substitution framework lacks safeguards for vulnerable populations. We're seeing real risks."
Financial Impact and Future Outlook
The Department of Health and Social Care (DHSC) allocated £1.8 billion for substitution initiatives in the 2025-26 budget. This includes money for community diagnostic hubs, digital health tools, and workforce training. The Office for National Statistics projects the pharmaceutical substitution market will grow 8.3% annually through 2028.
But there's a warning. The King's Fund analysis in June 2025 found that without fixing workforce gaps, substitution could worsen health inequalities by 12-18% in deprived areas. In Greater Manchester, initial substitution efforts widened care gaps before targeted interventions helped. "We fixed it," said one local health official, "but it took months of extra resources."
Looking ahead, the NHS 10 Year Plan aims to substitute 45% of hospital outpatient appointments with community or virtual care by 2030. That would require 15,000 more community healthcare professionals. If done right, it could save £4.2 billion. But if not? The Nuffield Trust warns it might increase overall system costs by 7-10% due to fragmented care and safety incidents.
Frequently Asked Questions
What does "dispense as written" mean on a prescription?
"Dispense as written" (DAW) means a doctor has specifically requested the pharmacy give the exact branded medicine listed, not a generic alternative. This happens when a patient has a bad reaction to generics, or when the branded drug is medically necessary. Pharmacists must follow this instruction unless there's an emergency.
How do Digital Service Providers (DSPs) work?
DSPs are pharmacy contractors required to deliver all NHS pharmaceutical services remotely. They handle prescriptions electronically-no face-to-face consultations at physical pharmacies. Patients order medications online or by phone, and DSPs ship them directly. This replaces the old system where you'd walk into a pharmacy to get your prescription filled. The 2025 reforms made DSPs the only way to access NHS pharmaceutical services.
Why is the NHS moving care to community settings?
The NHS is moving care to community settings to reduce hospital overcrowding, cut costs, and improve patient access. Hospital care is expensive and often unnecessary for routine issues. Community-based care-like home visits, local diagnostic hubs, or virtual check-ups-is cheaper and more convenient. The government's 2025 mandate specifically says "move care from hospital to community" to make the system more efficient and patient-friendly.
What are the biggest risks of these substitution changes?
The biggest risks are workforce shortages, patient safety issues, and worsening health inequalities. Many rural areas lack staff or infrastructure for community care. Remote dispensing has led to more medication errors in some areas. And low-income or elderly patients often struggle with digital tools, creating access gaps. Without proper support, these changes could harm vulnerable groups instead of helping them.
How will these changes affect prescription costs?
For most patients, prescription costs won't change much-generic drugs are already cheaper. But the 2025 reforms removed tax credit exemptions for some prescription costs and travel expenses. This means certain low-income patients now pay for medications they previously got for free. The NHS says this is temporary while new support systems are built, but it's causing real financial strain for some families right now.
Johanna Pan
February 6, 2026 AT 07:05This is a great step forward for healthcare! Definately a positive move. Although there are challenges, we can work through them. Let's stay optimistic. The NHS is making smart changes to improve access. We need to support our healthcare workers through this transition. It's important to remember the bigger picture. These changes will help more people get the care they need. Let's keep an open mind and work together. It's a big change but necessary for the future. We'll get through this together. The shift to digital services is inevitable, and it's time we embrace it. Many countries have successfully implemented similar systems. It's all about adapting and improving. We must not let fear hold us back from progress.
Gregory Rodriguez
February 7, 2026 AT 00:23Oh, fantastic! Another 'innovative' plan that'll probably make things worse. 'Remote dispensing'? Yeah, because nothing says 'healthcare' like a robot handing out pills. Can't wait for the chaos. They're just trying to cut costs and call it progress. I'll believe it when I see it. Maybe they'll finally fix the system... or maybe not. Either way, I'm not holding my breath. This is why we need better leadership. Or maybe not. Who knows? It's all just a game anyway.
lance black
February 7, 2026 AT 17:11This is the future!
Bella Cullen
February 7, 2026 AT 18:29Meh.
Cole Streeper
February 9, 2026 AT 05:30This is a government plot to control our meds! DSPs are 'Dreaded Surveillance Providers'. They're taking away our freedom. Mark my words-this is the first step to total control. They don't care about us. Just trying to control everything. Wake up people!
divya shetty
February 9, 2026 AT 22:23This policy is ill-conceived. The NHS must prioritize patient safety over cost-cutting. Remote dispensing without proper oversight is dangerous. We must halt this immediately.
Dina Santorelli
February 11, 2026 AT 20:21Ugh, another disaster in the making. They don't care about real people. Just pushing through changes without thinking. So tired of this.
Nancy Maneely
February 13, 2026 AT 01:16OMG this is a total disaster! They're destroying healthcare! How can they do this? This is why America is better. #SOS #SaveOurHealthcare
Phoebe Norman
February 13, 2026 AT 19:05The substitution framework lacks adequate safeguards for vulnerable populations as per BMJ. Workforce shortages are critical issue. Infrastructure gaps in rural areas will exacerbate disparities. Need comprehensive solutions.