Vasculitis: Understanding Autoimmune Inflammation of Blood Vessels
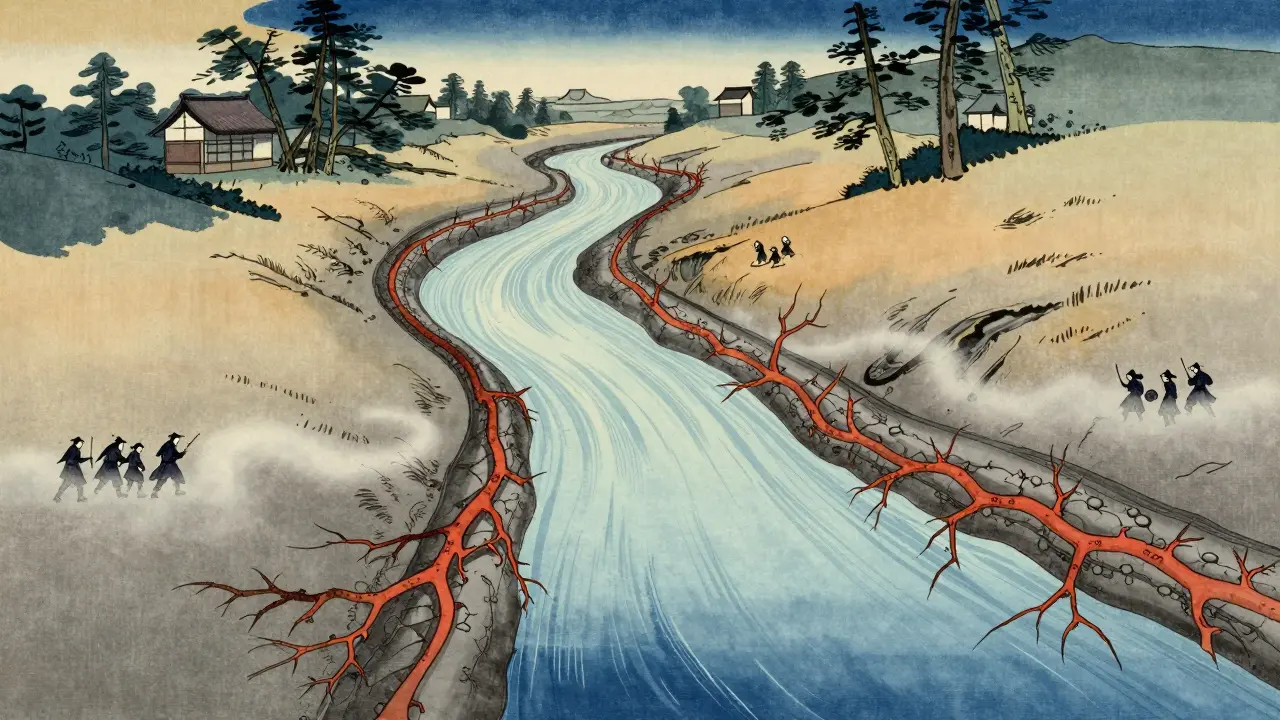
When your immune system turns on your own blood vessels, things go wrong fast. Vasculitis isn’t just one disease-it’s a group of rare autoimmune conditions where your body attacks the walls of your arteries, veins, and capillaries. This inflammation can narrow, block, or even burst vessels, starving organs of oxygen and causing damage you might not notice until it’s serious. Think of it like rust eating through a water pipe: early on, you don’t see it. But eventually, the flow stops-or worse, the pipe bursts.
How Vasculitis Works: Your Immune System’s Mistake
Your immune system is designed to fight off germs, not your own tissues. In vasculitis, something triggers it to see blood vessel walls as foreign invaders. The exact trigger? Still unclear. But once it starts, immune cells swarm the vessel walls, causing swelling, thickening, and sometimes destruction. This can lead to clots, aneurysms, or complete blockages. The result? Tissue death in the organs those vessels feed-kidneys, lungs, nerves, skin, even your brain.Types of Vasculitis: Size Matters
Doctors classify vasculitis by the size of the blood vessels it hits. That’s not just for labeling-it tells you what organs are at risk and how urgent treatment needs to be.- Large-vessel vasculitis affects the aorta and its big branches. Giant cell arteritis (GCA) hits people over 50, often targeting the temples. Headaches, jaw pain when chewing, and sudden vision loss are red flags. Takayasu arteritis mostly affects younger women and can cause weak pulses in the arms or high blood pressure from narrowed arteries.
- Medium-vessel vasculitis includes polyarteritis nodosa (PAN), which targets medium-sized arteries in the kidneys, intestines, and skin. Kawasaki disease, seen mostly in kids under 5, inflames coronary arteries and can lead to heart problems if not treated quickly.
- Small-vessel vasculitis is the most common and dangerous group. Granulomatosis with polyangiitis (GPA), formerly called Wegener’s, attacks the lungs and kidneys. Microscopic polyangiitis (MPA) does similar damage but without the granulomas. Eosinophilic granulomatosis with polyangiitis (EGPA), or Churg-Strauss, shows up with asthma, high eosinophils, and nerve damage. These are often tied to ANCA antibodies-anti-neutrophil cytoplasmic antibodies-that are key diagnostic markers.
What Symptoms Should You Watch For?
Vasculitis doesn’t have one signature symptom. It mimics everything from the flu to arthritis. That’s why it often gets missed for months.- Unexplained fever, fatigue, or weight loss
- Purple or red spots, bumps, or bruises on the skin-especially on the lower legs
- Joint pain or muscle aches
- Numbness or weakness in hands or feet
- Coughing up blood or shortness of breath
- Stomach pain, diarrhea, or bloody stools
- Headaches, vision changes, or jaw pain when chewing
- High blood pressure or reduced pulses in limbs
Some people feel fine until a kidney test shows protein in their urine-or an X-ray reveals lung nodules. That’s why doctors stress: if you have persistent, unexplained symptoms across multiple systems, get checked.

How Is It Diagnosed?
There’s no single test for vasculitis. Diagnosis is a puzzle made of clinical clues, blood tests, imaging, and tissue samples.- Blood tests show high inflammation: ESR over 50 mm/hr or CRP above 5 mg/dL are common. ANCA testing helps identify GPA, MPA, or EGPA. c-ANCA targeting proteinase-3 is 80-90% specific for GPA.
- Imaging like CT scans, MRIs, or angiograms can show narrowed or bulging vessels. For giant cell arteritis, a temporal artery ultrasound or PET scan can reveal wall thickening.
- Biopsy is the gold standard. Taking a small piece of affected tissue-skin, kidney, lung, or temporal artery-shows immune cells tearing through vessel walls. In skin vasculitis, you’ll see leukocytoclastic debris (broken-down white blood cells) around the vessels.
- Urine tests are critical. Even if you feel fine, protein or blood in urine can mean kidney involvement, which is a major red flag.
The Five Factor Score helps predict outcomes in polyarteritis nodosa: if you have kidney, heart, gastrointestinal, or neurological involvement, your risk of death rises sharply. Early detection saves lives.
Treatment: Turning Off the Immune Attack
Treatment depends on the type, severity, and organs involved. The goal? Stop the inflammation fast, then keep it off for good.- Corticosteroids like prednisone are the first line. High doses are used at first-sometimes up to 1 mg per kg of body weight-to knock down the immune response quickly.
- Immunosuppressants like cyclophosphamide or rituximab are added for severe cases. Rituximab targets B-cells, which produce the harmful antibodies. It’s now preferred over cyclophosphamide in many cases because it’s safer long-term.
- Avacopan, approved in 2021, is a game-changer. It blocks a key part of the immune system (C5a receptor) without the side effects of steroids. In trials, patients on avacopan had 2,000 mg less cumulative steroid exposure over a year.
- Tocilizumab, an IL-6 blocker, is now approved for giant cell arteritis to help reduce steroid use and prevent relapses.
- For Kawasaki disease, high-dose IV immunoglobulin and aspirin are used immediately to prevent coronary artery damage.
- For Buerger’s disease (a form of vasculitis linked to smoking), quitting tobacco isn’t just advice-it’s the only treatment that works. Keep smoking, and no drug will help.
Treatment usually lasts 18 to 24 months. Even after symptoms disappear, relapses happen in up to 50% of people with ANCA-associated vasculitis. That’s why ongoing monitoring is non-negotiable.
Prognosis and Long-Term Outlook
With early treatment, 80-90% of people with ANCA-associated vasculitis go into remission. But remission doesn’t mean cured. Many face flare-ups years later. The Five Factor Score predicts survival: someone with no major organ damage has a 95% five-year survival rate. With two or more major issues, it drops to 50%.Kidney failure, lung damage, strokes, and heart attacks are the biggest threats. That’s why regular blood pressure checks, kidney function tests, and lung imaging are part of lifelong care. Children with Kawasaki disease need echocardiograms for years to watch for coronary aneurysms.

What’s New in Research?
Science is moving fast. Researchers are looking for better ways to predict flares before they happen.- BAFF and MCP-1 are being studied as biomarkers in blood and urine to spot early signs of relapse.
- Mepolizumab, used for severe asthma, is showing promise in EGPA, cutting relapse rates by half in early trials.
- Abatacept, a drug used in rheumatoid arthritis, is being tested for giant cell arteritis to reduce steroid dependence.
The big shift? Moving away from heavy steroids. New drugs like avacopan mean fewer side effects-less weight gain, bone loss, diabetes, and infections. That’s huge for quality of life.
Why Diagnosis Takes So Long
Most patients wait 6 to 12 months before getting a correct diagnosis. Why? Symptoms look like common problems: flu, arthritis, asthma, or even depression. Doctors don’t always think of vasculitis because it’s rare. But if you have multiple unexplained symptoms-especially if you’re over 50 or have persistent kidney or lung issues-push for a rheumatology referral. A rheumatologist is the specialist who sees these patterns.As one expert put it: "Vasculitis is treatable, but early intervention may be needed to avoid significant, irreversible organ damage."
Can vasculitis be cured?
Vasculitis can’t always be cured, but it can be controlled. Most people go into remission with treatment and live normal lives. But relapses are common, especially in ANCA-associated types. Long-term monitoring and maintenance therapy are essential to prevent flare-ups and organ damage.
Is vasculitis hereditary?
No, vasculitis isn’t directly inherited. But some people have genetic traits that make their immune systems more likely to overreact. Having a family member with an autoimmune disease might slightly raise your risk, but it’s not passed down like a gene disorder.
Can stress cause vasculitis?
Stress doesn’t cause vasculitis, but it can trigger flares in people who already have it. The root cause is immune dysfunction, not lifestyle. However, managing stress helps overall immune balance and can reduce the frequency of flare-ups.
Do I need to avoid certain foods with vasculitis?
There’s no special vasculitis diet. But if you’re on steroids, you should limit salt and sugar to avoid high blood pressure and weight gain. If you have kidney involvement, your doctor may recommend a low-protein or low-potassium diet. Always work with a dietitian familiar with autoimmune conditions.
Can I still exercise with vasculitis?
Yes-exercise is encouraged as long as it’s gentle and approved by your doctor. Walking, swimming, and light strength training help maintain muscle, circulation, and mood. Avoid intense activity during flares. Listen to your body: if you feel unusually tired or short of breath, rest.
What happens if vasculitis is left untreated?
Untreated vasculitis can lead to permanent organ damage. Kidneys can fail, lungs can bleed, nerves can be destroyed, and aneurysms can rupture. In severe cases, it’s fatal. Early treatment dramatically improves survival and prevents disability.
Wendy Claughton
January 17, 2026 AT 13:55Wow. This is one of those posts that makes you stop scrolling and just... breathe. 🤯 I had no idea vasculitis could look like the flu for months before it hits you like a truck. My aunt had GPA and they missed it for a year-she lost hearing in one ear before they figured it out. Please, if you’re feeling off in multiple ways, don’t let doctors brush it off. It’s not ‘just stress.’
Jay Clarke
January 19, 2026 AT 07:32Oh here we go-another ‘rare disease’ post from someone who watched one episode of House. Everyone’s got ‘vasculitis’ now. You got a headache? Must be giant cell arteritis. Your foot’s tingling? Oh no, it’s ANCA-associated! Chill out. Most people with random symptoms just have Lyme or fibro. Stop Googling and go play outside.
Jake Moore
January 19, 2026 AT 10:14Actually, Jay, you’re missing the point. This isn’t hypochondria-it’s awareness. ANCA vasculitis has a 50% relapse rate even after remission. And avacopan? It’s real. I’m on it. Steroids wrecked my bones and mood for 2 years. Avacopan cut my prednisone dose by 80% in 6 months. No more moonface. No more insomnia. It’s not hype-it’s science. If you’ve never had to live with this, maybe don’t dismiss it.
Joni O
January 20, 2026 AT 01:15Thank you for this!! I’ve been waiting for someone to explain this clearly. I was diagnosed with MPA 3 years ago and honestly? I thought I was gonna die. But with rituximab + low-dose steroids, I’m hiking again. Just… please, if you’re reading this and have weird symptoms-don’t wait. Get that urine test. Even if you feel fine. Kidneys don’t scream until it’s too late. 💪❤️
Ryan Otto
January 21, 2026 AT 17:27Let’s be honest: vasculitis is not a natural disease. It’s a manufactured condition by Big Pharma to sell immunosuppressants. The real cause? 5G radiation, fluoridated water, and mRNA vaccines altering endothelial cell signaling. Why do you think the FDA approved avacopan so quickly? Because they need to replace steroids with something more profitable. The Five Factor Score? A statistical illusion designed to scare patients into lifelong drug regimens.
Max Sinclair
January 22, 2026 AT 13:07I appreciate how thorough this is. As a nurse who’s seen three cases in my 12 years on the floor, I can say this: early diagnosis saves limbs, kidneys, and lives. The hardest part isn’t the treatment-it’s getting someone to believe they’re sick when they look fine. If you’re reading this and your doctor says, ‘It’s probably nothing,’ ask for an ANCA panel. It takes 15 minutes. And if they say no? Go to urgent care and ask for a rheumatology consult. You’re worth it.
Praseetha Pn
January 23, 2026 AT 12:38OMG I KNEW IT!! This is EXACTLY what I’ve been saying since 2021! Vasculitis is caused by the government’s microchip implants in vaccines that activate neutrophils via quantum resonance! I had it! I had it bad! My legs turned purple and I could taste metal! I cured myself with turmeric, infrared sauna, and chanting mantras at 4am! Everyone needs to stop taking pharmaceutical poison and go back to nature! Also, did you know the WHO is hiding the cure? They don’t want you healthy!
Andrew McLarren
January 24, 2026 AT 20:31While the clinical presentation of vasculitis is indeed heterogeneous and often insidious in onset, the diagnostic criteria and therapeutic advancements referenced herein are supported by a robust and evolving evidence base. The introduction of targeted biologics such as avacopan and mepolizumab represents a paradigm shift in management, significantly reducing glucocorticoid burden while maintaining disease control. It is imperative that primary care providers maintain a high index of suspicion for multisystem inflammatory syndromes, particularly in patients presenting with constitutional symptoms and unexplained organ dysfunction.
Andrew Short
January 25, 2026 AT 22:02People like you are the reason medicine is broken. You’re out here treating vasculitis like it’s a yoga retreat. ‘Just get a urine test!’ Yeah, and then what? You get labeled ‘chronic’ and stuck on immunosuppressants for life. You think these drugs are safe? Tell that to the 40-year-old who got fungal pneumonia from rituximab. Stop spreading fear. Most of these people don’t even have vasculitis-they have anxiety and bad diet. Quit hyping up rare conditions to sell fear.