Visual Dosing Aids: Syringes, Droppers & Measuring Tools for Safer Medication

Visual Dosing Aid Simulator
Medication errors cost lives every day, especially when patients or clinicians have to measure liquids under pressure. Imagine trying to draw the right amount of epinephrine in a chaotic emergency - a tiny mis‑step can be the difference between recovery and tragedy. Visual dosing aids were created to cut that risky guesswork by turning numbers into clear, color‑coded visuals that anyone can read in seconds.
What Are Visual Dosing Aids?
Visual Dosing Aids is a family of medication‑administration tools that rely on visual cues-large markings, colour zones, and intuitive scales-to guide users toward the correct dose. They emerged from a bitter awareness that medication‑related adverse events were alarmingly common, prompting researchers like Callens et al. (2009) to design a pediatric antiretroviral aid that matched dosing to a child’s weight band without complex calculations.
Key Types of Visual Dosing Aids
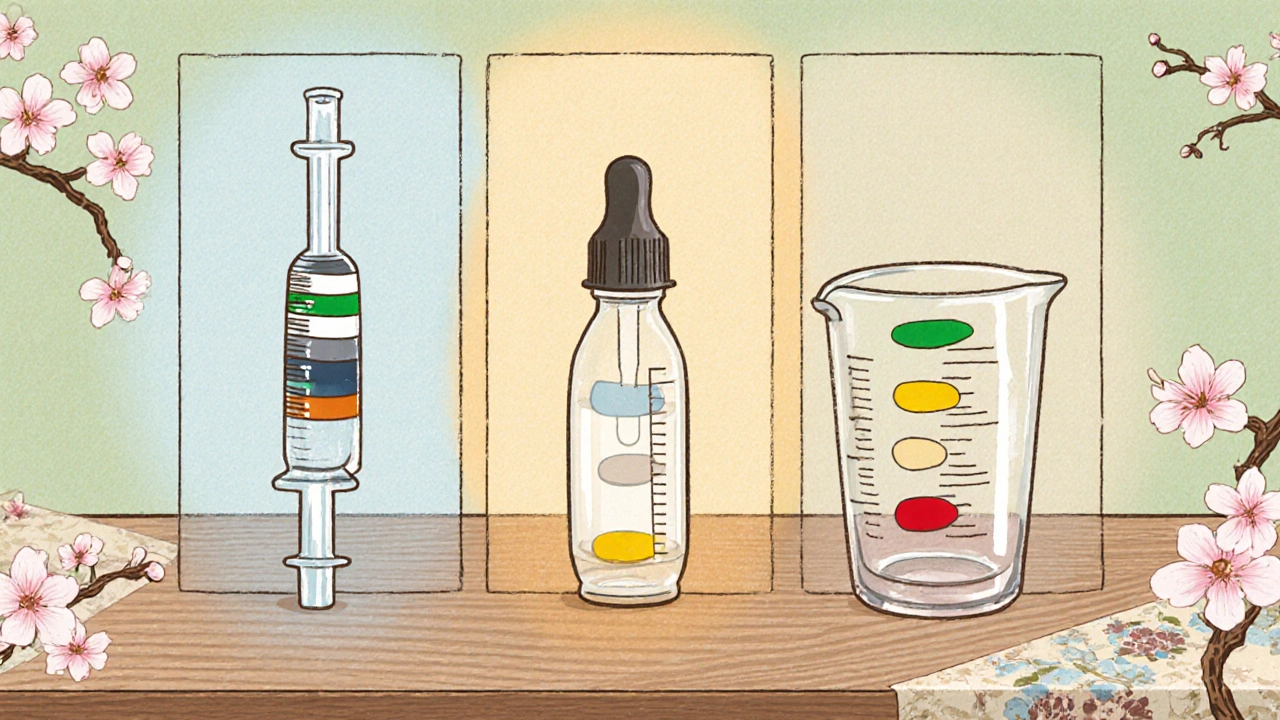
Three tools dominate the market today, each tailored to a specific delivery method.
- Syringe is a precision device that draws liquid medication into a barrel and releases it through a needle or catheter. Visual syringes sport enlarged numbers, contrasting colour bands, and sometimes a single‑step scale that skips unnecessary graduations.
- Dropper is a plastic or glass instrument that dispenses medication drop‑by‑drop, often used for eye or ear drops. Modern droppers include a transparent window that fills only when the target volume is reached, and some even change hue as the dose fills.
- Measuring Cup is a wide‑mouth container calibrated in millilitres with clear demarcations for common doses. They frequently employ colour‑coded zones (safe, caution, high) to warn users before they over‑fill.
How Visual Dosing Aids Reduce Errors
Research consistently shows that visual aids shrink both the rate and speed of mistakes. Gardner et al. (2018) ran a contrast‑medium reaction simulation with 138 radiology participants. Teams using visual aids made dosing errors in only 18.2% of cases, compared with 40% for the control group. Moreover, they administered intramuscular epinephrine 36.2% faster (97 seconds vs. 152 seconds).
The study also revealed a confidence boost: 97.8% of participants said the visual aid made them feel more certain about the dose and route. That psychological edge matters because stress amplifies the likelihood of slips.
In pediatric settings, the Visual Dosing Aid designed for antiretroviral therapy eliminated the need for manual weight‑based calculations. By simply aligning a weight band with a colour stripe, clinicians could instantly read the correct millilitre volume, cutting calculation errors that historically plagued low‑resource clinics.
Implementing Visual Dosing Aids in Clinical Settings
Adopting visual tools is easier than you might think, but a few practical steps keep the rollout smooth.
- Assess Workflow Gaps. Identify high‑risk points-emergency medication rooms, pediatric wards, and home‑care kits.
- Choose the Right Tool. Match the device to the medication form (e.g., syringes for injectable drugs, droppers for ophthalmic solutions).
- Provide Brief Training. Even an eight‑minute simulation usually suffices because the design is intuitive. Emphasise colour‑code meaning and how to verify the dose.
- Integrate Into Protocols. Update standard operating procedures to reference the visual aid explicitly. The Institute for Safe Medication Practices recommends documenting the aid as part of the medication‑verification checklist.
- Monitor & Iterate. Track error rates post‑implementation. If self‑administration errors persist, consider adjunctive measures like double‑check or digital reminders.
Resistance often stems from habit. Highlight the data-over‑50% error reduction-and let early adopters share success stories to build momentum.
Choosing the Right Tool - Quick Comparison
| Feature | Syringe | Dropper | Measuring Cup |
|---|---|---|---|
| Typical Use | Injectable meds (IM, IV) | Eye/ear drops, oral liquids | Oral liquids, irrigation |
| Visual Cue Type | Enlarged graduations, colour bands | Transparent window + colour change | Milimetre marks + colour‑coded zones |
| Accuracy (± ml) | ±0.1 ml | ±0.2 ml | ±0.5 ml |
| Training Time | 5 min | 3 min | 4 min |
| Cost (USD per unit) | 0.30 - 0.60 | 0.10 - 0.25 | 0.20 - 0.45 |
| Best For | Emergency injectables (e.g., epinephrine) | Home‑care eye drops, neonatal meds | Oral antibiotics, nutrition formulas |

Best Practices & Tips for Safe Medication Administration
- Never Rely Solely on Memory. Keep the visual aid within sight of the medication container.
- Check Colour Zones Before Administering. Green usually means ‘safe dose’, yellow prompts double‑check, red signals overdose risk.
- Confirm the Correct Concentration. Some tools are calibrated for specific drug strengths; using a 10 mg/ml epinephrine with a tool set for 1 mg/ml will still mislead.
- Use Two‑Person Verification for High‑Risk Drugs. Even with visual aids, a second pair of eyes catches lingering slips.
- Document the Aid in the Medication Record. The The Joint Commission lists visual verification as a safety checkpoint in its National Patient Safety Goals.
Future Trends: Going Digital Without Losing Simplicity
While today’s visual aids are mostly analog, manufacturers are prototyping smart syringes that flash a coloured LED once the correct volume is drawn. Early pilots show a further 10% drop in error rates, especially for self‑administered drugs like auto‑injectors. However, the core principle stays the same-clear, immediate visual feedback that anyone can interpret without a phone or tablet.
Regulators are catching up, too. The Institute for Safe Medication Practices is drafting guidelines that would require all new injectable kits to include a visual dosing component by 2027. If you’re planning a medication‑safety program, now is the perfect time to embed these tools and stay ahead of compliance.
What makes a visual dosing aid different from a regular syringe?
A visual dosing aid adds large, high‑contrast markings and colour‑coded zones that instantly tell you if you’re in the safe range. Regular syringes have tiny numbers that are easy to misread, especially under stress.
Can visual aids be used for oral liquid medications?
Yes. Measuring cups designed with colour bands and clearly spaced millilitre markings are a form of visual dosing aid for oral liquids, soups, or pediatric suspensions.
Do visual dosing aids work in emergency situations?
Absolutely. Gardner et al. (2018) showed that participants using visual aids administered epinephrine 36% faster and with half the error rate compared to standard tools.
Is special training required to use these tools?
Minimal training is enough-most designs are intuitive. An eight‑minute simulation usually covers colour‑code meanings and correct alignment.
Are visual dosing aids recommended by safety organizations?
Yes. Both the Institute for Safe Medication Practices and The Joint Commission cite visual verification as a key strategy to cut medication errors.
Suzanne Carawan
October 25, 2025 AT 18:48Oh great, another colourful plastic tube promising to save lives-because we all know doctors love reading tiny numbers under stress.
Octavia Clahar
October 30, 2025 AT 07:16I really appreciate the push for safety, but let’s be honest: we’ve seen countless “simple” tools turn into a new source of confusion for patients and overburdened nurses alike. The intention is solid, yet the real‑world rollout often feels rushed, leaving clinicians juggling extra steps instead of saving time. Still, I think the color‑coded approach has merit if we pair it with proper hands‑on training.
Lionel du Plessis
November 3, 2025 AT 20:43The device integrates visual ergonomics, calibrating ml increments with chromatic indexing, enabling rapid dose confirmation.
Andrae Powel
November 8, 2025 AT 10:10Totally get where you’re coming from, Octavia. In my experience, a brief hands‑on demo-just five minutes-can turn those “confusing” tools into second nature. When staff see the green‑yellow‑red zones in action, confidence spikes, and error rates dip noticeably. It really is all about that quick, focused training session.
Leanne Henderson
November 12, 2025 AT 23:36Lionel, love the tech‑speak! What’s even cooler is that these visual cues can be introduced without a massive overhaul-just a few stickers and a quick walkthrough, and you’ve got the whole ward on board, ready to dose safely, efficiently, and with a splash of colour that actually helps.
Megan Dicochea
November 17, 2025 AT 13:03Andrae’s point about short demos hits the nail on the head but let me add that the real challenge is sustaining those gains over weeks and months especially when staffing shifts and new hires come on board they often miss the original brief training and revert to old habits which is why continuous visual reminders and periodic refreshers are essential to keep the safety net tight and effective
Jennie Smith
November 22, 2025 AT 02:30Wow, these tools are like the superhero capes of medication administration-bright, bold, and ready to rescue!
Let’s get them everywhere.
Anurag Ranjan
November 26, 2025 AT 15:56Exactly, Jennie – a quick demo and they’re ready to roll.
James Doyle
December 1, 2025 AT 05:23When we talk about medication safety, the moral imperative is crystal clear: we cannot accept a system that places patients at risk for the sake of convenience. The data presented here, showing a drop from 40% to under 20% error rates, is not merely a statistical footnote; it is a clarion call for systemic change. Visual dosing aids embody the principle that simplicity can coexist with precision, and this should become a non‑negotiable standard across all care settings. It is unconscionable that, in many institutions, budgetary constraints still delay the adoption of such low‑cost, high‑impact tools. Emergency departments, where seconds matter, should prioritize these aids to ensure that epinephrine and other critical drugs are delivered flawlessly. Moreover, the color‑coded zones align with human cognitive strengths, reducing reliance on fragile memory under duress. By integrating these tools into protocols, we honor the duty of care owed to every patient, especially the most vulnerable pediatric population. Do not let complacency erode the progress we have witnessed. The ethical responsibility rests on administrators, educators, and clinicians alike to champion these aids and embed them into everyday practice. Failure to do so would betray the trust placed in us by those we serve.
Edward Brown
December 5, 2025 AT 18:50James makes a noble point, but let’s not ignore the hidden agenda behind the push for visual aids. The same manufacturers that sell us these “safety” tools also lobby for stricter regulations that lock hospitals into proprietary systems. It feels like a subtle way to control the market while claiming to improve patient outcomes. Keep your eyes open.
ALBERT HENDERSHOT JR.
December 10, 2025 AT 08:16Edward, your cautionary stance raises valid concerns about market dynamics. It is essential, however, to balance vigilance with the undeniable benefits that standardized visual cues bring to clinical practice. By fostering transparent procurement processes, we can mitigate potential conflicts of interest while still advancing patient safety. 😊
Kala Rani
December 14, 2025 AT 21:43Sure, because adding a rainbow to a syringe is the ultimate solution.
Donal Hinely
December 19, 2025 AT 17:48Kala, if we’re going to paint everything pink and call it progress, at least make sure it works-stop sugar‑coating the flaws and get real about implementation.