Lactic Acidosis: What It Is and Why It Matters
Lactic acidosis sounds scary, but it’s basically a build‑up of lactic acid in your blood that makes the pH drop too low. When that happens, you can feel sick fast – like a sudden wave of fatigue, nausea, or rapid breathing. The condition shows up in emergencies, after intense exercise, or when certain medicines or illnesses mess with how your body handles sugar.
Understanding the basics helps you act fast. If you or someone you know has risk factors – such as diabetes, liver disease, or heavy alcohol use – knowing the warning signs can be a lifesaver.
Common Causes
Most cases start when cells can’t turn glucose into energy the usual way. That forces them to use a backup pathway that creates lactic acid. Here are the top triggers:
- Severe infection or sepsis: Your body’s fight response can flood the bloodstream with chemicals that raise lactate.
- Intense exercise: Sprinting or heavy lifting can push lactate levels up, but it usually normalizes quickly.
- Medications: Some cancer drugs, metformin (especially in kidney problems), and certain HIV meds can tip the balance.
- Medical conditions: Liver failure, heart failure, and shock reduce oxygen delivery, leading to a lactic surge.
- Alcohol binge: Drinking a lot in a short time overwhelms the liver, causing extra lactic production.
Often, more than one factor stacks up. For example, a diabetic patient with an infection and a new drug is at higher risk than anyone alone.
How to Spot It
Symptoms don’t always look the same, but a few patterns repeat:
- Feeling unusually weak or tired even after resting.
- Nausea, vomiting, or stomach pain.
- Fast, shallow breathing – your body tries to blow off carbon dioxide to raise pH.
- Confusion or a “cloudy” mind, especially if blood pressure drops.
- Muscle cramps or a burning sensation during light activity.
If you notice these signs and have a risk factor, call a doctor right away. Blood tests will measure lactate; levels above 4 mmol/L usually signal an issue, and higher numbers mean more urgent care.
Doctors also look at other lab values – like kidney function and blood sugar – to figure out the root cause. The faster they know what’s driving the acid build‑up, the quicker they can treat it.
Treatment focuses on three things: stopping the source, flushing out the acid, and supporting the organs that are struggling.
For an infection, antibiotics are the first step. If a medication caused the rise, the doctor will pause or switch it. Intravenous fluids are a staple; they dilute lactic acid and improve circulation. In severe cases, a bicarbonate drip may be needed to raise blood pH, but it’s used carefully because it can cause other imbalances.
People with chronic conditions should keep a close eye on their health. Regular check‑ups, proper medication dosing, and staying hydrated can cut down the chances of a sudden spike.
Bottom line: lactic acidosis is a red‑flag response—your body’s way of shouting that something’s wrong with its energy balance. Recognize the symptoms, know the common triggers, and get medical help fast. Early action often means a quick recovery and prevents complications.
Metformin and Alcohol: Understanding the Lactic Acidosis Risk
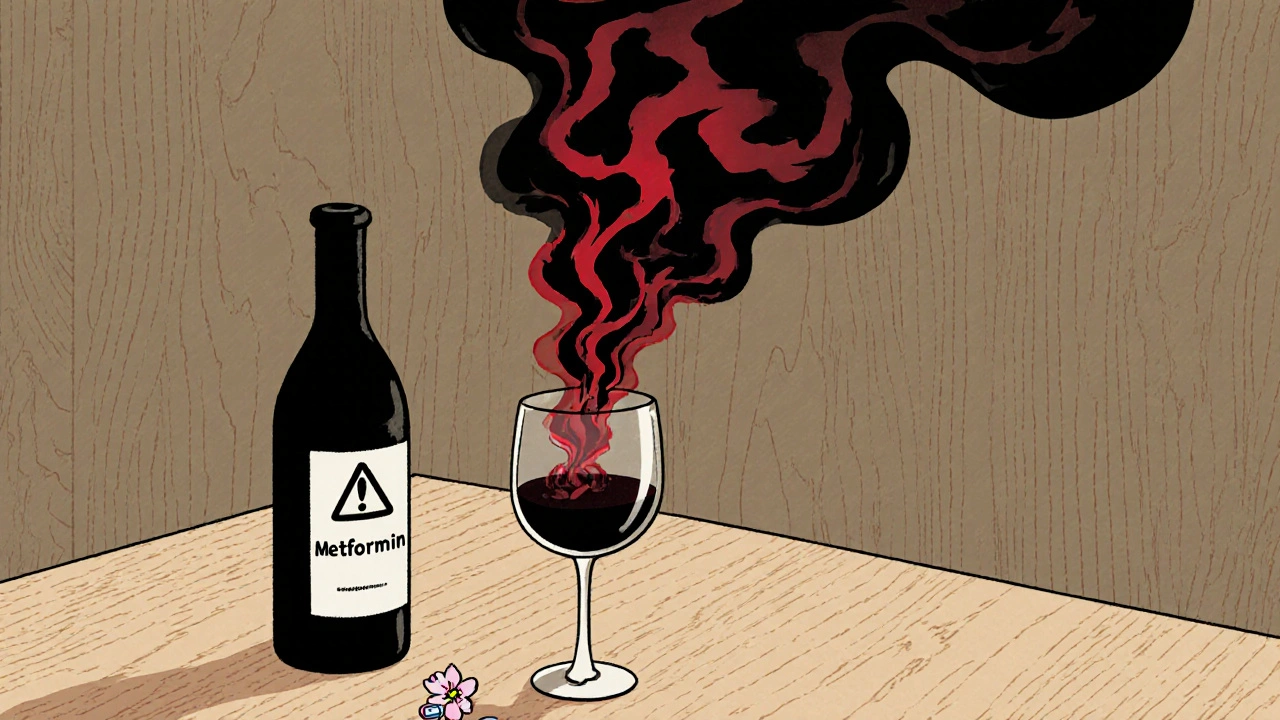
Metformin and alcohol together can trigger lactic acidosis-a rare but deadly condition. Learn the real risks, warning signs, and what to do if you drink while taking this common diabetes medication.
Sitagliptin‑Metformin and Alcohol: Risks, Precautions, and Safe Use

Learn how sitagliptin‑metformin interacts with alcohol, the health risks involved, and practical steps to stay safe while managing type2 diabetes.